|
Dementia-Friendly Vision Expanded for State and National Implementation
By M. Ellenbogen
January 2016
PREFACE
As a person living with younger-onset Alzheimer's disease I find it a challenge these days to be able to share all my thoughts with groups of people. While I appear to be very normal when we have short talks, there are many issues that I struggle with. I have lost the sharpness and quick response needed to be able to interact with you all at your level. .While I may not respond immediately, answers come to me many hours later. Sometimes they never do. When I hear conversations I do not hear the entire sentence but part of it, and in my mind I fill in the blanks. It's weird to know I have many answers in my head, but cannot find a way to retrieve them.
Because of all this, I want to ensure I have the opportunity to share my vision of what I would like to see happen in the U.S. and globally. Some of these ideas come from others who have created them before me, while many are my own or a combination of both.
The original document from 2013 has already been shared with many world leaders. This is a current, updated version that includes some new material. I did have assistance in the editing of this compilation, which I hope you will use to advance my dementia-friendly vision wherever you live.
AWARENESS, EDUCATION & CONSOLIDATION
AWARENESS & EDUCATION
For those of us living with younger-onset Alzheimer's disease (YOAD), the public's lack of awareness and understanding is a huge barrier to our ability to sustain full and meaningful lives. Awareness of YOAD is needed to change public perception of who gets Alzheimer's and other dementias. Young people who are under 30 can get it. I know of a 29 year old and a 30 year old who have it. Our country must use commercials, billboards and posters in key places to make the public understand that not everyone living with dementia is in their 70s or 80s. The faces representing the disease must change! We must show younger people in a multi-media campaign so the public learns that Alzheimer's is a disease that affects all ages; it is not just associated with getting older.
Similarly, the public's lack of awareness and understanding about Alzheimer's disease and other dementias must change. Alzheimer's is often used for any form of dementia. While Alzheimer's represents approximately half of the types of dementia, there are other forms of dementia as well. An estimated 1.4 million of the over 5.2 million Americans living with dementia have Lewy Body dementia (Lewy Body Dementia Association, 2015). Other common forms of dementia include vascular and fronto-temporal dementia. The Dementia Action Alliance recommends the term 'dementia' as the appropriate inclusive term.
Currently people who have Alzheimer's and other dementias cannot be cured. There is no way to slow the progression of the disease, and most die within 4 to 8 years of diagnosis. While these two statements are strong I feel this is what it's going to take to reach younger generations and others to jump in and help. We cannot beat around the bush; the public needs to know that this is a horrific way to die. Death is slow and painful, not to mention the impact it has on the family. Organizations like the Alzheimer's Association and others need to provide information about all aspects of this disease so people can be better prepared if or when they or a loved one is diagnosed with dementia.
REMOVING THE STIGMA
We must remove the negative stigma associated with the disease. Too many people are ashamed to let others know that they have this disease. They act like they did something wrong to get it. Now is the time to join me, come out of the closet, hold your head up and be proud in making a difference in how we are looked upon by others and ourselves. We need to show that we are still capable of doing many things at our own pace. We must be able to live life to the fullest even though we have the diagnosis.
CONSOLIDATING IDEAS FROM AROUND THE GLOBE
Most of the people I speak to at high level do not know what Dementia Friendly Communities (DFCs) mean. They act like they know until I put them on the spot to explain. Not many will do that, but I need to know people understand; they need some kind of a blueprint to help guide them to start the process.
I will start out by saying I do not believe anyone out there has it right yet and it will probably also continue to evolve over time. What they all lack is to see what is needed it because we focus on it from a silo point of view and are not willing to place the demands on what are truly needed. We tip toe around it with many of our requirements so that others buy in. While they are doing great things in Japan and the UK I am still not sure someone has clearly written the definitions of what it all means and all who are involved.
A lot of what Act is doing in the US is copied from those programs. I also believe it is not getting the same level of involvement as the UK but it is certainly a great start. Olivia M. needs to be careful on how hard they push and ask. The Act model has now been kicked off in the US as Dementia Friendly America. I think we should have high level standards and allow people to choose what level they are willing to support. We should start off by combining the best of programs used by world leaders.
What I believe we need to do is to create a new temporary group. That group should only consist of the people from around the world who created their own DFCs. One complete manual should be created by including every single idea that they all came up with into one manual. Have a separate section for why they changed direction and what had failed and why there was a need for change in direction or modification to their programs. What are the ideas they would like to see added since their implementation that never made it. Even if they do not think it is possible. Once we have this list then we can eliminate duplication. They should all vote on it as the ongoing model. They also need a few people with dementia. I do not mean just bodies but people who really have a good view of what is really happening. I also believe we should create tiers or levels for the various goals created. Maybe 6 levels with the 6th one that we may know will never even happen. But maybe some parts will. That will be our way to measure progress and give other bragging rights and create competition. We can talk further but I believe you know where I am headed with all this. A 1 may be as just a simple awareness to all of the communities to know about dementia. Just knowing. It seems like such a simple task.
In my opinion people like ADI should be behind this and other national groups like AARP. That is the only way we will focus to work together and not create silos. I realize it will need to be done at many local levels but we need to do it with global thinking in mind
For further information about Dementia-friendly Communities:
DEMENTIA-FRIENDLY COMMUNITIES
My vision of a dementia-friendly community is a bit involved, but if it is implemented it will have a huge impact in many ways. When I think of a dementia-friendly community it refers mostly to those who are in the early to mid-stages of the disease. This idea was first started in the UK by my friend Norm McNamara who is living with Lewy Body Dementia.
We need to encourage dementia-friendly communities and businesses in which dementia is treated like any other disability.. This community should include first responders, health providers, service providers, local businesses, public transportation providers, airports, and the public..
UNIVERSAL SYMBOL: THE WORLD PURPLE ANGEL
There is a common logo that is slowly becoming the internationally known symbol for those living with dementia and I think we should use it. It is called the World Purple Angel.
 To be used on all websites and dementia patients information and hospitals To be used on all websites and dementia patients information and hospitals
 For stores and businesses to show they know and have been educated For stores and businesses to show they know and have been educated
This was created by N. McNamara and is starting to get a lot of recognition. In fact it is now going to be used in some US hospitals as an indicator that the person has cognitive issues; they hang it on the door of the hospital room of the patient. I recommend that we adopt this symbol for all programs connected to dementia-friendly communities. Many people create their own logo for their own local area. For some reason they all want to be different. I see that as a huge mistake. When people with dementia leave their area they should be able to rely on a symbol that is used everywhere they go. Since many already have a symbol they should also include the World Purple Angel along with their own. This will be the same as for people who rely on a handicap sign. We must do this if we are truly looking to help people living with dementia. While I don't care which symbol is used I think we should not create a new one. The World Purple Angel is already known in all 7 continents. For that reason alone I would say that is why we should focus on using that symbol. Also it was not created by any organization, but people living with dementia.
Each of the following elements should be considered in the creation of dementia-friendly communities:
MEDICALERT & SAFE RETURN SERVICES
Six in 10 people with dementia will wander and/or get lost. A person with Alzheimer's may not remember their name or address, and can become disoriented, even in familiar places. Anyone who has memory problems and is able to walk is at risk for wandering. Even in the early stages of dementia, a person can become disoriented or confused for a period of time. It's important to plan ahead for this type of situation. Wandering and getting lost can happen during any stage of the disease. Be on the lookout for the following warning signs:
- Returns from a regular walk or drive later than usual
- Tries to fulfill former obligations, such as going to work
- Tries or wants to "go home", even when at home
- Is restless, paces or makes repetitive movements
- Has difficulty locating familiar places like the bathroom, bedroom or dining room
- Asks the whereabouts of current or past friends and family
- Acts as if doing a hobby or chore, but nothing gets done (e.g. moves around pots and dirt without actually planting anything)
- Appears lost in a new or changed environment
For people with dementia wandering is dangerous, but there are strategies and services to help prevent it. First responders need educating, and a system needs to be created that will help identify us without becoming a target for others. I believe we need a system that allows individuals to register with the state, or someone of equal standing, this should include care partners as well as it's important to have emergency info on the caregiver. I would like to see something similar to MedicAlert at a state level. What follows is a brief outline of the MedicAlert system:
MedicAlert® + Alzheimer's Association Safe Return® is a 24-hour nationwide emergency response service for individuals with Alzheimer's or a related dementia who wander or have a medical emergency. We provide 24-hour assistance, no matter when or where the person is reported missing.
- If an individual with Alzheimer's or a related dementia wanders and becomes lost, caregivers can call the 24-hour emergency response line (1.800.625.3780) to report it.
- A community support network will be activated, including local Alzheimer Association chapters and law enforcement agencies. With this service, critical medical information will be provided to emergency responders when needed.
- If a citizen or emergency personnel finds the person with dementia, they can call the toll-free number listed on person's MedicAlert + Safe Return ID jewelry. MedicAlert + Safe Return will notify the listed contacts, making sure the person is returned home.
The Alzheimer's Association has developed training tools and support programs to prepare law enforcement, EMTs, fire fighters and other first responders when they encounter a person who is wandering.
The information on your medical alert bracelet will connect health professionals with your emergency medical information. We provide memberships and services designed to protect you and your loved ones during a medical emergency or time of need.
MedicAlert's medical bracelets, medical IDs, and other medical jewelry have been used to alert responders of the underlying medical conditions a patient may have -- such as allergies, anaphylaxes, diabetes, and autism. First responders are trained by MedicAlert staff to recognize all forms of medical IDs, and our services ensure they get your up-to-date medical information, the moment they need it, to make informed decisions about your treatment and care. MedicAlert services and medical IDs are also used to communicate advance directives and can even help those with Alzheimer's or dementia make it home safely during wandering emergencies.
For more information please visit their website: http://www.alz.org/care/alzheimers-dementia-safety.asp.
Those who choose to register would wear a bracelet similar to the one above or some type of tag on a chain. By registering the people would be able to take advantage of many benefits. Family would need to register and could be set up when in the clinic for diagnosis as well as info bracelet ordered and resources given out.
All those registered would be given a unique identification number that will have basic information that could be used in case of emergency. To stop the system being abused or compromised, this information should only be accessible by the relevant people, following a secure procedure and calling a special telephone number and providing the person's ID number. (This would only be accessed by calling a provided number)
It may include information like blood type, allergies, last wishes, drug information, doctors, emergency contacts, and addresses,
This system needs to be linked with the 911 systems, and the yellow dot program. When a person calls the fire department the address should be flagged immediately when it comes up as a person with dementia living in the residence they are being dispatched to. This is important for many reasons.
A person with dementia may panic in this situation and may not know how to respond to the emergency conditions. They may be much worse than a child in some cases, and just curl up in a corner in fear and just stay there. They may not even speak out when people are calling their name. They may have even started the fire and are scared. They could be combative and the firefighters need to know how to deal with that situation. There are many other reasons why the firemen need to be aware before arriving.
If we ever have some kind of a natural disaster or need to evacuate for some emergency this system will be a major asset, especially for those who may be at home on their own. By being registered this will 9 insure a much better outcome for those who may not be able to think for themselves. Many of these people would not leave with just a simple call and they may not even understand what is said in robo-call type alerts.
If the police are called that should also be flagged immediately. It could be the person with dementia calling in, and not able to articulate the problem. It could even be a false alarm because they are scared when there is really no threat. Sometimes people with dementia have been known to make serious accusations of being threatened by their spouse with a gun, which has led to spouses being locked up for days because the system was not aware of the person's dementia. Again, if members of the emergency services are coming to a house where a person with dementia resides, they need to treat threats in a completely different way otherwise it can escalate and even become deadly.
Not everyone will easily display, or even be willing to wear the bracelet or tag because of the stigma surrounding this disease. Only when this changes will people feel more comfortable about sharing their diagnosis with others.
Throughout this document I give many examples to where one can wear a product to be identified as a person living with dementia. Keep in mind if we do this right it will only require one if we can all learn to work together and make it a seamless operation. I have no doubts that can work and that is my intent.
ISSUES WITH POLICE: DRIVING & WEAPONS
Driving
Driving laws need to change to remove the licenses of those that are no longer capable, while not impacting those that are still able to drive. It should be based on the person's true driving experience and ability, and not on perceptions or fears. It should have nothing to do with getting lost; GPS tracking devices can help us if that is a concern. Many people have the misconception that if a person with AD is in an accident the insurance company will not pay for the claim, or may even sue them. While there are many tests available to test one's driving, many are not fair to a person living with AD. In fact if the average person was given the same test they may even fail. Better tests that deal the individual living with the disease are needed and all must be able to test this test. Some of the cognitive tests do not correlate to driving ability, but to failing and singling out people with AD. That is completely unfair. For example I fail the Trail-Making Test, Part B and I still drive very good. The testing should be free or paid by insurance. These tests can cost around $300 -$350, and provide annually. Every 2-3 months we should drive with a spouse or other person who understands us to see how well we drive. That should be a regular part of our future lives, and they should be the ones to tell us when they feel it is time to give up driving. I am not saying that people with AD should not eventually stop driving, but it should be done for the right reasons -- that they will become a danger to them or someone else. What we need to 10 focus on are the real problems of driving, and not the side issues related to them. We must embrace new ways to deal with people with AD and find new opportunities and technologies to use to our advantage so we can enhance the lives of those with this disease; so they can continue to lead a normal life for as long as possible. Do not fall into the one-size-fits-all trap because all those living with AD are different from each other and we must figure out a way to make everyone feel safe including those living with the disease. We are still human beings. My biggest fear is that one day I will have an accident and my license will be taken away. It may not have anything to do with my Alzheimer's, but it will be perceived that way. I have had 3 to 4 car accidents in my lifetime, some being my fault while most were others. We all have them.
As a person living with AD I seem to notice much more. I see many people run through lights, not use turn signals or come to a complete stop at the stop sign. I see people cut others off or shift in to other's lanes without paying attention. All I can think is that if people saw me do any of these things they would want to take my driver's license away, yet all of these folks are normal and they just get a free pass. Why?
If someone with Alzheimer's is stopped for a sobriety test they may fail because they have trouble following instructions or poor gait. They may also be much slower with their responses, and may even give you a blind stare because they are confused. They may not be able to follow complex directions. Directions need to be broken down into steps.
I know we want to make the roads safe so we need better testing methods for Alzheimer's patients who drive. Be prepared to deal with people who may seek help when they are lost. We can get lost while driving; this does not mean we cannot drive. These two issues are often confused by many.
The car should also have some sort of identification mark. It could be tied-in with the yellow dot system; however, I am concerned that we may become a target because of that. We are much more gullible because of this disease and that could be a very serious issue. I was someone who always kept all those scammers at a far distance, and now I am starting to fall prey to some and think it will only get worse as time goes on and I get worse. It could be on a driver's license, like a donor or class B license. It could be a code that is not obvious to all.
Weapons
While I am on the subject of issues with police there is a document, which I shared with the chief of police a few years ago. While some changes are being implemented in some parts of the US, I am not sure they are being addressed in PA. I tried to reach out to my local police department and training facilities, but was just blown off. One of the biggest and most serious issues that I feel needs to be addressed is that of weapons. I came very close to taking my life, and even told a police officer on the telephone, but he refused to do anything. I just wonder how many other people pleaded for help and ended up killing themselves because nobody answered their cry for help. This is unacceptable.
Sometimes people with dementia get confused or feel threatened and may make accusations that could land someone else in jail. Be prepared to deal with cases like this. They need to be handled very differently from someone without dementia. Some would say like a mental illness. They believe what they are saying is fact.
Alzheimer's patients can sometimes become very aggressive and defensive during an argument, they can even become threatening. This is the wrong time to try to remove them from their home. They need to be calmed down first; otherwise it can become a disaster for that person, because many will not understand what is going on.
We require a place to store or remove guns from a home when needed . I came up with a simple way that this could be accomplished without too much impact on the police. A gun safety device can be used to secure the guns in the person's home, and the key can be given to someone responsible. There were other suggestions made.
TECHNOLOGY TO ENHANCE QUALITY OF LIFE
In preparation for the 2015 AARP Dementia Care Technology and Innovation Forum, I wrote the following: These are ideas I have shared with others over the years.
I believe technology is critical to those living with dementia and their caregivers. But I want to emphasize that it needs to be very affordable or better still, free.
I would like to tell you a little about me. In my past jobs I worked in IT, Data Communication, TV & Radio repair and also did programming. I designed and built world class data centers. All of my life I came up with ideas that most though were impossible and the demands I made were unreachable. I can tell you almost all of them became real at a later time. And I have had some crazy ideas.
There are many different technologies already available that, once modified, will be suitable for someone with dementia.
Here are a few ideas.
A simple type pressure + mercury type sensor, which is addressable, could have multiple applications, such as keeping an eye on your loved one at night if they get up, or used on a door in the house to trigger an alarm.
Timers specially designed for electric stoves that can be programmed to operate during certain hours with automatic shut off during certain times of the day.
Special water sensors that can be added to every sink that will trigger automatic water shut off in case of overflow.
GPS use for tracking and wandering needs improvement. Battery life and service area are two key areas. The price today is unaffordable. There should be a special class of pricing for these types of devices when it comes to monthly fees.
RFID is a great tool in combination with GPS. Products can be made to just work around the house at no monthly cost.
We make alarm systems that have all kinds of sensors in the house which all report back wireless to one centralized controller. Why are we not looking to do that with all products for dementia? When I had a boat I had many gadgets on board and I was able to connect them all together so each on could coordinate with each other and give me the information I needed when necessary. That is how we should be thinking; a standard protocol to use and interface to make it standard.
My idea is to have a noise canceling head set that has multiple uses. A head band with a pin point accurate direction mic that when facing a person it will pick up what they are saying and not the surrounding noise or people speaking. It should also be able to be used standalone noise canceling and MP3 input. Must be easy to use as this is for people with dementia. The biggest problems I and many living with dementia is that we can no longer filter sounds out. When we are in public and someone speaks it all comes in at the same volume all mixed together. If I could focus on the one person I would go out more frequently to restaurants and public places. Many times in public places the noise is so loud that I cannot stand to be there. We need to make these as small as possible and to be somewhat attractive.
There are many ides I have about using technology in assisted living centers or places like them. Sound proofing and design is critical to people living with dementia. Colors and lay outs are all extremely important, as is lighting.
A simple solution that is in place but needs to be enforced, TV commercials on some stations are much louder than the regular scheduled program. That is enough to set me off or create agitation.
While there are many types of apps they need to be made easier to use.
My GPS system for my car is great. If it only had a dementia mode that would tell me much earlier to start moving over toward the right lane if I want to get of further down the road. Especially when doing high way driving or very fast. Many times I may not hear it at first as I am concentrating, maybe a simple voice command that can be repeated if prompted. All of this is possible with additional programming and mode options.
A simple solution needs to be created for those of us who live with dementia. The governments need to sell us a single card or give it for free to be used unlimitedly on and transportation system. I have lots of trouble buying passes and often end up going the wrong. They need to find a way to keep us engaged by using these systems. I believe this should be part of a bigger system as I have spoken about in my dementia friendly communities.
Wearable sensors can become another great area because many of these ideas can be incorporated into one devise: reminder for pills, when too eat, appointments or even how to get home if lost; or if you fall or such, panicking. The idea and applications are endless.
Google glass is one such product that could have such a huge impact for those living with dementia. It could help me get around help me remember what people say to me if it was set up to do all that. It has many limitations today and laws need to change. You are not allowed to record conversations today in many states and that is critical to people like me. You should be able to speak to it and say I am lost I need help and it would automatically take action.
Packages for easy dictation from a portable recording device to a word document. There are some things available but they need enhancements.
For me my Outlook is my brain but it does not easily connect with any other devices. That should be easy for someone to allow it to sync up to today. I am good at home but lose the capability when it's not available to me.
Since I wrote my drone idea I have spoken with Project Lifesaver who will have something similar out soon. While I think what they have falls short and way to costly, that organization does some great things and should become embraced by all. That would not only save money but save lives. Let's work with them to improve their system with technology. Below was what I have shared with them and others.
Let's save lives and reduce potential injury for those who wander because of dementia, including Alzheimer's. The task of searching for wandering or lost individuals with cognitive conditions is a growing and serious responsibility. Without effective procedures and equipment, searches can involve multiple agencies, hundreds of officers, countless man hours and thousands of dollars. More importantly, because time is of the essence in such cases, every minute lost increases the risk of a tragic outcome. This is a program that must be offered in all our states. After all, we give prisoners bands to track them for house arrest with taxpayers' dollars. Why don't good people deserve to be kept safe? Statistics show it will save money and have better outcomes if we all invested.
I have an idea on how we can find people with dementia who wander in less than 30 minutes. What is even more interesting is it requires very limited staff and is mostly automated. While this may all sound futuristic I can guarantee you this is all possible with technology today.
Picture this, someone goes missing and someone calls the emergency services number. Immediately they are identified as a person with dementia, and the operator pulls up the person's identification number from a pre-established database. They ask the caller for the last known location of where the person was seen. They enter that in the computer and hit enter which starts a search.
At pre-set locations, automatic drones equipped with GPS and RFID technology take off in to the air over a 50-mile radius, which is equal to about 7854 miles. That number can be greater or less. The drones have software that allows them to talk to each other from drone to drone. Within 10 minutes they will identify if they have located the position of the person missing. This can go one of two ways. I have made the assumption the drone can only identify signals at 10 miles radius based on RFID technology. That number is more like 12 -15 miles. So that will cut down on the number of drones needed.
If the person is located it will send back GPS signals of the location of the person to a central computer, which will automatically dispatch the police to the area. They are equipped with a RFID tracker, which can locate the person if they are within two miles of them. They will then find the person based on the signal. The numbers I use are very conservative so in reality it will be even better.
If no signal is detected the computer automatically expands the search to a much wider area or in a specific direction. There are many factors that go into how fast one would initiate such expansions. If a medical concern exists one may do all at one time. This would all need to be determined.
According to my numbers we have 3.8 million miles in the US and would need 8,400 drones. For the PA State, which is 46,000 square miles, we would need 102 drones. While this number was purely picked out of my head I believe for $250.00 a drone could be built with all that is needed to accomplish all this. This would be one that is self maintained. I have many ides on that alone. I am not surprised if the military already has designs for these or even others planning already.
Some assumptions are made in order for this to happen. All people with dementia who want to be in the program will register with their local police. They will be given a bracelet to wear that will be multifunctional.
The cost of this may not even be as high as we think because we may be able to tap into the companies who are going to use this technology. Amazon, Google are just some. I cannot imagine these organizations would not be willing to add software that will help benefit the community.
I was told that it cost about $10,000 every time we do a search. Let's do this more efficiently and quickly while saving lives. I believe this could all be possible today. I also don't believe it would take a long time. It can be started in one state as a trial and then branch out. Keep in mind that this system can have even more uses if designed properly. It can be used for other things such as weather, tracking prisoners, locating vehicles, etc. There are many other uses which could lead to shared cost.
There is a small cost to the bracelets as they would need their batteries replaced. Some places already use such system.
This is another idea I have shared with others. There is no website out there that can help those that needed. This one will help all and could be good for other causes.
Over the course of the last 6 years I have had the opportunity to see many sites that are geared to helping those impacted by dementia. So many times I see these folks struggle to get the help they seek. What I find even worse is that many of these people who are so desperate for information get bad or misleading information because people are willing to share their ideas with others. You have people discussing a topic they are unfamiliar with giving someone else recommendations based on their own experience or something they may have learned.
What is so wrong is that we have no system in place to help these folks, which is frustrating because no one seems to want to create a system that will help all of those who use the Internet today. I have recommended this idea to many and no one seems to be interested in building a system, which in my opinion, would be a lifesaver to many.
In order to build this system it would require IT folks to work closely with dementia experts along with caregivers and those living with the disease.
I see this as a very simple solution and it must be made available at a well-known site, such as AA or a government site. The system would be based on what I call the Helpdesk approach, which is used by many IT organizations.
When you call a helpdesk they need to ask you the least amount of questions so they can quickly route you to the proper department responsible for your issues. Their goal is to fix it on the first try but if not they do the hand off. I believe this system works very good if you know to ask the right questions and provide good answers that lead to solutions.
Here is an example of how I see this application helping those with dementia. It will need to be created like a flow chart with the right questions and to continue to drill down until you get to the answers the people are seeking.
When you first come to the site it will have the first question. Who am I? You would then be given a number of choices such as: I am a caregiver, I am living with dementia, I am a medical person, I am with the press, I am a friend or family person of a person with dementia, or I am a business. You could have more or less and while these are not the right names this gives you an idea on how it works.
Based on your answer it will start to drill down to another level. Let's say you selected "I am a caregiver". That now brings up the following question. Why am I here? You would then be given a second set of choices such as: crises, general education, what's in the future, resources, emergency, and support group. Again this can be longer or shorter based on the categories one can think of.
Now that you made a selection it will drill down to one more level. Let's assume you selected "Crises". It will now ask you to make another choice. What type of issue do you have? Now it is going down to the third level, which will have many categories on topics. This must be much longer.
Some of those choices may be: suicide, swallowing, falling, behavior issues, wandering, grooming, sleeping, activities, legal stuff, hospital, assisted living centers, products, resources, helpline, and call in line, medications, and hospice. Again this list will be much longer.
Now some may drill down to one or two more levels but most will end at this level. This is where you will provide detailed answers to what they needed. This will be the most choice for the reason they came to this site. This should help them with the correct answers for why they are here. When they select titles of description it will give them all of the details on a specific subject.
Let's say you had selected "behavior issues". This will take you to only information related to issues for items related to deal with behavior issues only. It may include ways to deal with them, where to go to seek help. Different types of issues and possible solutions. Each area should have an option that says I do not see an answer for my issue. They need to always have a way for an answer.
I do believe much of the information already exist in databases that we can already use. Not all sites will have all the answers so there is a need to allow for the answer to be linked to another site.
There is absolutely no doubt that if we create this system it will have a huge impact to helping caregivers and others affected by dementia. This will lead to better quality of life to the individual with dementia but also a lot less stress to the caregivers. They will be able to get to the answers when they need them.
I have many ideas and always willing to work with anyone in beta testing. I believe technology can allow us to live life to the fullest if it is done right and affordable. If we have the right engineers in a room anything is possible as long as they are all willing to work together.
DEMENTIA-FRIENDLY HOSPITALS
Being an advocate for dementia has driven me not only to educate myself on the disease but also to investigate how the medical world responds to our needs and requirements. Over time I have learned a great many things, one of which is that the US healthcare system is not appropriately prepared for those living with dementia.
To date, people who are responsible for implementing change tended to look at the situation from the caregivers' point of view, which is another major issue that needs addressing. We never ask those who are living with the disease what they want or need and I feel no polices or procedures should be considered without input from us.
Health providers and institutions must change in many ways to make it better for those living with dementia. Physician education -- Doctors need to be better educated, and need to commit to a more timely diagnosis so that patients can collect the benefits they deserve and are entitled. Doctors should not act like our lives are over. Once a diagnosis is made it should automatically trigger a referral to a psychologist or psychiatrist so the person can learn to deal with the devastating news. Many people are in denial and waste that last few years not knowing what to do. Instead they should be living life to the fullest. Make the memories. We must be encouraged to make living wills and put our financials in order quickly since our minds are going. We have no time to delay. Encourage participation in medical trails and offer frequent checkups. Living wills should be very different for those with AD. While this is a taboo subject we should have the right to end our life in a dignified way. We must talk about these issues.
Below is a list of issues that I have been working on with a local hospital in hopes of starting the first dementia-friendly hospital in PA. I was trying to build a training program with the Alzheimer's Association along with a question and answer session with people like me who are living with the disease. Below is the list I have shared with them. Some hospitals are actually doing a quick cognitive test by asking 3 words upon registering to see if there may be a concern even if the person does not have a diagnosis. I would expect that all hospitals would educate staff on the issues, for instance we can easily get lost while trying to find a department as an outpatient:
At registration, identify a person that can and will be able to be involved in all decision-making, along with the patient.
At registration, identify a person that will be given full access to all records on behalf of the patient.
Patients bring in a list of current medications. If for some reason you must change the drug or dosage for any reason, the issue should be addressed with the patient and caregiver to ensure there are no issues (even if it's as simple as converting to a generic). Sometimes patients cannot take another form of the same drug-ask them.
Example: My doctor switched me to Galantamine rather than Aricept because of side effects. In the hospital, they substituted Aricept. (My wife had Galantamine with her, but of course it is a big deal that you should not take your own meds.)
A special ID bracelet should be placed on this type of individual so the staff is alerted that this patient has some form of dementia. This will help them if the patient is acting confused or wandering or just needs a little extra help or explanation. It may also mean that the patient isn't great at making good decisions. If you need a color, purple is perfect.
Example: I needed a Fleet's enema pre-op. The nurse asked if she should give it to me or if I wanted to use it myself in the bathroom. Of course, I offered to do it myself. I found I had difficulty once I got in the bathroom by myself; a bad decision on my part. The nurse should have not given me the option. (We do not want to appear stupid or show our flaws so we may do something to show we are still capable when we may not be.)
I know they always ask the patient for their full name and birthdate -- hat may be hard at times for us. I can become confused on a good day, in the hospital it can be worse because of pain medication or being awakened suddenly or the stress of just being out of our routine. Maybe another way can be figured out. (Before a nametag is placed on a dementia patient it may require 3 or 4 staff individuals to ask the patient for that information and each must identify the same information before the ID is placed. This will insure the wrong tag is not placed on the patient. Use the verbal ask on critical things like surgery and drugs given the first time the nurse may see the patient)
There are special things one needs to know about using Anesthesia. Anesthetic agents are a cause for concern in AD pathogenesis. Luckily, the field of Anesthesiology has addressed these concerns in an excellent and honest manner. I would defer to their consensus statement:
http://www.anesthesia-analgesia.org/content/108/5/1627.full
http://www.mc.vanderbilt.edu/
The bottom line seems to be to avoid isoflorane.
Do not always consider a patient being confused as a part of the dementia, but it could be much worse due to the drugs they are on. When I was on pain killers my wife could not even get a response from me that made much sense, and she knows what's normal for me.
A real concern exists on what type of drugs the patient may receive for Anesthesia. Pain killers will also have a much greater impact on this type of person.
While ordering food from a menu is simple, it is very overwhelming for me to keep track of things and what items may even go together, or are even needed. I will probably need help with this task.
Don't assume we can figure out how to use items in the room like TV, Phone, call button, and anything else. Please point them out and provide a simple explanation on their use.
Aides should not be the first point of contact. I am not always good at explaining what I need and the aide was not always good at interpreting what I was trying to say. Aides are okay for follow-up or to help with food menus. Again this is why training on all levels is so critical.
When asking a question, give them a minute or two to answer without going on to some other question. You could even ask them to think about it and come back in 5-10 minutes, no longer. This is very subjective depending on the person. We often need a few minutes to gather our thoughts. We might even answer a question right away and then realize a few minutes later that that wasn't what you asked.
Somehow you need to insure the patient response is really correctly given -- they sometimes give an answer just to not appear stupid or show they did not understand. Maybe some visual aid or clues can be given along with the verbal depending on the stage the patient is in.
Try to keep items and things in the room in the same place once they determine the best location for them.
I personally feel these patients should be kept a bit longer than the average person, for observation. This would just be to make certain there are no issues at time of release.
Offer a pen and paper to keep in the room. Tell them to write down questions they want to remember to ask when the nurse comes in the room.
Keep in mind many patients with dementia can no longer spell correctly and may use the wrong context for words.
This is the wristband that was implemented for all patients with dementia at Brooksville Regional Hospital, along with this square magnet to be placed on the outside of the patient's room on the doorframe. Before any of these wristbands will be used, training seminars from the Alzheimer's Association will held for all of the hospital staff members. This is a major step forward in maintaining the safety of all dementia patients during hospital stays.

The hospital loves the purple angel logo, They went through three different band designs before this. The problem being that purple is also the national color for DNR (Do Not Resuscitate).. What I love about it the most is that it's for "all dementias," which is what we truly need in the hospitals.
Patients should be made aware of the living wills which should be very different for those with AD. While this is a taboo subject we should have the right to end our life in a dignified way. We must talk about these issues.
Recommendations to DAA Optimizing Health & Well-being Workgroup Members:
Dear DAA Workgroup Members:
After listening to the call yesterday and having time to think about it, I probably need to say that I do not believe there are any well established procedures for the Hospital systems on how they should deal with patients with dementia. While I believe there are some great best practices that can be pulled from all over the world related to care nursing homes, and environments dealing with what people refer to as behavioral issues, there are none that I have seen today that do the same for hospitals.
I have a lot of material that I pulled together that I hoped to start a first of its kind tool. While I was partially successful I realized the bigger stumbling block was the time these people needing to spend on education and the cost of that to the organization. I have also learned that from dealing with the hospital trying to implement the plan, that there is a thirst for this knowledge and they are extremely uneducated concerning dementia. I was very surprised that staff did not even know what dementia was in relation to Alzheimer's. It was very scary to hear them explain what I consider to be the basics.
One of the biggest problems I faced is I have no credentials to get these people to listen to me. I had a team of educators who were willing to dedicate their time to help create the course for the hospital I was involved with. It was all free to them. They felt it would take 3 hours to do it right plus taking the virtual dementia tour. They decided to do it in 30 minutes plus the Dementia tour. The problem was they did not make it mandatory. The staff has about 5000 and that is no mistake. Based on what I last know it probably had 300-500 actually take it. Mandatory is the key. I also realized while the dementia tour was a eye opener it left people confused of not being able to truly make sense of it all. That is where I believe I added the most value. We had a question and answer session with a person living with dementia. That I believed was the biggest eye opener for them and to tie together what they had just went through. I only had two people that could not get the concept but were changing to think differently about it.
I believe what is needed is to create a module lesson plan that is web based that is broken down in 30 minute segments. It should consist of 6 lessons that they receive CEU credits for. This should be mandatory for all new hospital employees within 90 days of hire. All this would be considered part 2. Part 1 would be the taking of the dementia virtual tour followed by 2 -3 30 minute segments of a filmed question and answer period. The questions are the best questions taken from medical staff and answered by the person living with dementia. There is so much to be gained from all that. Only after taking part 1 can someone take part 2. The other item of key importance is the ability to identify patients with dementia upon admission. I have information on ways to accomplish this within the HIPAA requirements.
The biggest problem I see with all this is the Virtual dementia tour. This is a bit more involved and requires live people to make it happen each time it needs to be implemented. Studies have shown that this must happen first to get the most of the education. I have many great ideas on how to make this all successful and many Dementia educators agree with what I have in mind. It would just take someone's time to spend time to speak with me and to convey it to others to make the best possible plan.
I have seen the Alzheimer's Association Plan and it even falls short. I heard it from their own high level people. They are doing something in Florida that is kind of good in the hospitals, but I believe it falls short. It was driven by someone who was a caregiver and they were looking at it from their viewpoint. It is good but failed to see it from my eyes as a patient.
I also am aware of a few organizations out there that one gets certified for taking their courses. I honestly can say I have not seen the material. There are only a few and they charge money for them. The very first question I have is who gave these people the right to say the have the best knowledge to educate us all and to claim they can give us a certification. They were very smart marketing people in my view and found a niche. I even asked one of the CEO if they had someone with dementia in the process and they were quick to respond they had caregivers involved. I told them that they had failed already in the process. In my last communication with them they were going to bring it up to their Board as they thought that was a good idea. I find it sad that these people are considered leaders and did not even think of something so simple.
In my opinion if we want to bring change we cannot focus at the hospital level. If we want quick change we need to go after places like the above and places like The Joint Commission, and others like them that provide accreditation. We need to work with them to insure they have the best model and they can help make it successful. I tried to do this early on but I have no credentials in their eyes. I think they probably laughed at me.
With this group and the support of some key doctors, part of DAA, I believe they may be willing to listen. I have had 3 stays in the hospital and all I can tell you is the system is broken for people with dementia. My recent stay at the hospital was after they had supposedly implemented some training. They had failed in my eyes as they totally failed me as the patient. It's one thing to not know what you do not know, as is the case with most hospitals today. But it's another when they do know the issues and fail to address them. So I guess what I am saying is we need to create the actual training material as I do not believe it exists today.
DEMENTIA-FRIENDLY BUSINESSES
Work environments should be created in which we can still feel productive without penalty to the employer or the person living with the disease.
I envision that businesses take a 2 or 3 hour course provided for free by the Alzheimer's Association and others, to make them aware of the issues that people with dementia deal with, and what they may need help with. On completion of the course they will get a sticker that they can display in their place of business that says Dementia-Aware with a picture of the logo. By doing this we will be creating awareness, and educating many on how to make it easier for us to still function as members of society; something that is not always easy when you are an adult who is facing progressive cognitive challenges.
Some of the issues may be
- feeling panic in a large store when becoming separated from the person they came with
- being asked a question and not being able to respond, or even giving the wrong information
- having trouble locating items in stores
- no longer being able to calculate how much they have spent or can spend if they have a budget
- getting lost, losing sense of direction, or not being able to locate the car in the parking lot
- it would be nice to get assistance when there are similar products to choose from, because I can no longer do comparison shopping based on price, or if an item in the same category is on sale
- When it comes to purchasing tickets for travelling on trains etc. staff need to be aware that we may need help. We may not be able to check in at the airport unaided. We should not be penalized for not being able to take advantage of online offers because we cannot use computers. We may need to be taken to a gate or to a temporary room until our flight or train is ready (this does not mean we need to be ferried about in a wheelchair!)
Even though we are living with AD we should be encouraged to live life to the fullest. We need to keep our minds engaged. We should be able to do volunteer work, and to still do high level functioning jobs, and the company not be penalized, and the person with the disease should not be penalized by Social Security because they are working. As volunteers I would expect that our transportation expenses be paid for, and maybe even lunch. This will have a positive impact on the people with the disease and be of great benefit to a company that can utilize the person. Some do not want jobs like pushing hospital beds around, or doing simple tasks when we have a high function skill set.
Companies need to treat dementia like any other disability. The following comments are from an individual who works in Human Resources:
"Tell your story to HR Management. What kind of company do they want to be? How will they protect their human resource that has dementia - and be good risk managers by taking appropriate action to minimize the risk of litigation for wrongful termination under ADA? What are the costs of unrecognized dementia in employees i.e., lost productivity, errors, quality, odd/unexplained behavior, a decline in management skills leading to more of the above? What are the State percentages? Give examples -- If they are a company of 1,000 employees that equates to xx employees who will have early onset dementia -- can they afford to be blind to the problems these individuals will cost the organization? Alzheimer's is not all about the needs of the caregiver. Little to no attention is given to the INDIVIDUAL WITH DEMENTIA. If the company has a PEP program (Personal Employee Program that typically provides 8 to 12 sessions of counseling when an employee suffers from personal problems (divorce, runaway kids, elderly care, etc.) why not have a Dementia Hotline/Exploration. Why not help people self-diagnose early and assist them to seek a medical diagnosis, so TOGETHER the employee and company can make a plan for them to ultimately exit from the company with dignity - example: an employee is still skilled, but may need to move from having the responsibility of being a manager to becoming an individual contributor. Why wait to FIRE someone for non-performance, when you could continue to employ the person until the day comes where there is no job which matches the employee's skills. A diagnosis of dementia IS protected under ADA. Why wait to be sued by an employee who was unfairly terminated because of his disability. Why not be proactive and humane, keep the person off unemployment; mitigate your exposure to litigation. Such a small cost to set up a program to assist and empower employees to work TOGETHER with them, give them dignity and determine together when it is time to go. Help them transition to retirement with disability; unemployment; assistance from the Alz Association."
I would like to see a simple pamphlet be put together for those who are living with the disease covering all the benefits available to us living with dementia. It must be simple to understand, short and to the point. The procedure should include all of the resources available and where one should turn. Today one has no clue and they do not know what is available. This should be handed out with a diagnosis from your doctor.
Laws need to change so those who are getting fired can collect the benefits they deserve. Let's stop burdening the social security system. Because there is no clear test for the diagnosis of YOAD, many diagnoses are delayed. Many people are terminated from jobs, and are unable to collect their long-term disability insurance, because of the two-year law. Most diagnoses occur much later, as in my case. I paid a lot of money into a long-term health disability plan in my company and I lost it all because of the law. I now get less than a third of what I would have been entitled to, and no medical coverage which I would also have had, all because of a law that does not work for individuals with this disease. Changes must be put in place until we have better tests available. If someone is terminated for non-performance and they have been diagnosed with dementia at a later time, they should have the right to go back at least six years to prove their case. Companies should not get a free pass because we all pay for this injustice. The two year law is a failure for people like me with dementia.
I was terminated from my job before I got a diagnosis which took another 6 years. Now I am forced to rely on government disability. Dementia is a disease, and the people who have it should be treated that way.
FINANCIAL ISSUES & NEEDED SYSTEM CHANGE
Younger-onset Alzheimer's, also known as early-onset Alzheimer's, generally refers to those who are affected by the disease before the age of 65, usually in their 40s or 50s. Because of their younger age and healthy appearance, doctors often attribute symptoms of Alzheimer's to depression or stress, resulting in delayed diagnosis. These symptoms, such as challenges with short-term memory, impaired judgment and difficulty making decisions, eventually progress to a point where they affect workplace performance, and ultimately, jeopardize employment. Many individuals living with younger-onset Alzheimer's are in their prime earning years and supporting loved ones at home. The loss of income and access to employer-sponsored health benefits can be devastating.
This document reflects State and Federal issues that may not be working. My goal is that if the existing jurisdiction responsible is not able to enhance the process, the other will step in and fill in the gaps so people are not impacted. It is my hope that they can work together to fix the weaknesses in the system that may have been overlooked.
To help address their financial need, many individuals with younger-onset Alzheimer's rely on Social Security Disability Income (SSDI), or Supplemental Security Income (SSI). In March 2010, the Social Security Administration (SSA) added early-onset Alzheimer's to its Compassionate Allowance Initiative, which expedites the disability determination process and serves as a trigger to begin the two-year wait for Medicare benefits for those under the age of 65. Family members (e.g. spouses and minor children) may also be eligible for benefits based on the applicant's work record. This addition by SSA has been a huge relief for individuals and families dealing with Alzheimer's.
However, many are treated like they are crooks when they apply for Social Security Disability. It creates an added burden on the family and the patient. People say that the Compassionate Allowance act will help people, but it did not help me, and many keep saying that it's not working.. The following story is from an ongoing case. This program may be better but the people who run the programs are clueless in many ways on what a person with AD can or cannot do. This person is not only struggling financially, but has no one to look out for them. I cannot even imagine the hell they must be going through because it would take me forever to complete the same forms.
-------------------------------------------------
It's so nice of you to think of me. I wanted to add that the reason I was turned down on the first application and reconsideration was because I filled out the RFC form myself (I lived alone at the time and it was a necessity) and not for lack of medical evidence. My son now lives with me but only minimally supervises me and does the driving. An examiner at Social Security took it upon himself to send out an investigative unit because he felt I must be faking Alz even though in the course of the application and reconsideration, I saw 5 doctors, 4 of whom thought I had Alz disease and 1 CE examiner who thought it was possible but hesitated because I still have average intelligence (my IQ was in the 140s when I was in graduate school and now around 100, which I think this is an alarming decline). This SAA evaluator then proceeded to imply that all the doctors I saw were fooled. He even sent out an investigative unit to actually videotape me without my knowledge (following me to one my CE appointment one day and sending undercover police officers to my home the following day). I don't remember the investigators coming to my home and didn't see them at the hospital (obviously quite good at the stealth part). At the hospital, the doctor walked me out to the lobby because he was afraid I would get lost said a few minutes later I "disappeared (I got my ride, of course)." They went back to the doctor looking for me, and he apparently was very concerned I had actually gotten lost in the hospital. At my house, they said I walked slow to answer the door but I didn't limp (???) and was polite and had my hair combed (implying I was not disabled based on my outward appearance and probably less than 30 seconds of conversation). The evaluator felt that anyone who could describe their symptoms on an application, write mostly coherently, (though always needing multiple edits, spell check, and entailing a lot of repetitiveness) answer the door, use a phone, live alone, or drive in the early stages had to be faking it regardless of MRI, neurological tests, etc., that clearly gave me a diagnosis of EOAD. Long-winded, I'm sorry. I'm still feeling kind of abused and outraged. As for now, my lawyer thinks he can get me a hearing OTR and I'm hoping for that and a favorable decision If not, it will be another 12-15 months before I have a hearing date, this because the SSA evaluator apparently does not understand that earlystage Alzheimer's is not immediately visible on the surface. In the meantime, I am now in the process of selling my home to live with my adult son as we can no longer afford the upkeep (this is a modest home -- but now far above my means).
I'm very lucky that my son is living with me to help, but it means I do not qualify for Medicaid because his income is now considered my income and puts us just above the income limit. He can't put me on his insurance as I don't qualify as a dependent because of my small LTD policy, which in turn needs to be repaid to the insurance company if I do get SSDI. I've gone from a single, self-supporting middle class woman, to lower middle class, now to poverty level in the course of about 4 years. Without my son's help, I'm probably within 3 months of living on the street. At the same time, I'm suddenly placing a tremendous burden on him and fouling up his goals in life.
Another note: I find it ironic that my neurologist tells me to exercise vigorously, take care of my health, and socialize as much as possible in order to function longer whereas I sense the government is telling me that I'm not eligible for disability insurance (despite working since age 13 and paying into the system for years) unless I give up, lie in bed, and wait to die.
-------------------------------------------------
It would be great if the Alz Assoc could find a way to educate the SSA evaluators on what Alzheimer's disease looks like in younger people in the early stages so that other people don't go through what I'm going through now. It would also be great if they could lobby for earlier Medicare benefits (rather than the 2 year wait after SSDI) for all disabilities that are only going to deteriorate.
Once we have a diagnosis, we should all be entitled to the same level of benefits no matter what our age is. One should not be impacted by other laws that were not designed or intended for those living with this type of disease. There are many state and federal programs that limit us from being able to contribute to or benefits we are not entitled to because of our age. Family savings should not be wiped out just because one has dementia. A family should have a cap on what they must payout. Why should the surviving spouse be left penniless because their partner was sick? Is it enough that most of us have already had to deal with financial hardship we were not accustom to? Pa. Caregiver Support Program: care recipient/household income must be @ 200% of poverty or below for max. reimbursement.
Below are just of a few of the ways this disease is costing me more money than ever:
I once did most things around the house and now I have to rely on others and the cost is adding up very quickly. Many things are becoming neglected which will have a greater cost in the long run. I used to be good at comparison-shopping and now I no longer do it because I cannot recall the price so I can compare. This has such a huge impact from food, gas, utilities and everyday items.
Furthermore, under the Patient Protection and Affordable Care Act (PPACA), individuals with a pre-existing condition receiving SSDI can join high-risk insurance pools and receive immediate health insurance coverage while they wait for Medicare benefits to become available. This has been particularly helpful for those who are unable to find affordable health insurance because of their Alzheimer's diagnosis In addition to the cost of care, Alzheimer's imposes an immense burden on families. Last year, there were an estimated 671,000 unpaid dementia caregivers in Pennsylvania, providing 765 million hours of unpaid care valued at over $9.3 billion. Unfortunately, the physical toll of caring for Alzheimer's also resulted in over $472 million in additional healthcare costs to unpaid caregivers in your state. To assist those who care for people with Alzheimer's in Pennsylvania, the state offers the Pennsylvania Caregiver Support Program. Preference is given to caregivers of care recipients who are 60 years or older, but eligibility was recently expanded to include care recipients who are 18 years or older. All care recipients must demonstrate functional limitation and financial need.
Regrettably, age is still a barrier to other support programs for individuals with younger-onset Alzheimer's and their caregivers. All caregiver support programs that receive funding under Title III of the Older Americans Act require care recipients to be at least 60 years or older. Likewise, Pennsylvania's Medicaid 60+ waiver and aging block grants are only available to those who are at least 60 years old. Restricting eligibility by age, rather than diagnosis, forces many families affected by younger-onset Alzheimer's to exhaust their own resources and put their own health and financial security at risk.
Health providers and institutions must change in many ways to make it better for those impacted. Physician education -- Doctors need to be better educated, and need to commit to a more timely diagnosis so that patients can collect the benefits they deserve and are entitled. Doctors should not act like our lives are over. Once a diagnosis is made it should automatically trigger a referral to a psychologist or psychiatrist so the person can learn to deal with the devastating news. Many people are in denial and waste that last few years not knowing what to do. Instead they should be living life to the fullest. Make the memories. We must be encouraged to make living wills and put our financials in order quickly since our minds are going. We have no time to delay. Encourage participation in medical trails and offer frequent checkups.
Living wills should be very different for those with AD. While this is a taboo subject we should have the right to end our life in a dignified way. We must talk about these issues. We must encourage research and provide funding. In order to eradicate this disease we need to find more sources of funding and redistribute current government funding to bring Alzheimer's to a level comparable to other disease research. Trials need to provide more flexibility by using technology. Many are unable to participate due to lack of flexibility. Some people do not participate in clinical trials because they feel it will not help them. They need to know that it's not about them but what they do can help someone in their family should they get the disease. Since a cure may be long in coming, it would also be nice to see more funding provided to investigate treatment methods to maintain independent function longer. The drug companies have taken the stage and it's all about what increases their profit and not necessarily about what will help the patients.
Make government grant programs free, fair and balanced -- Some researchers using government research grants are discriminating by age and minorities because of rules being set forth by both the provider and the receiving researcher. This will prevent the formation of an accurate picture of this disease. For example, black people are twice as likely to get Alzheimer's. Why?
Eliminate the term Caregiver - Come up with a new term for the word caregiver when used for people in the following stages
- Very mild decline
- Mild decline
- Moderate decline.
We find it very demeaning and do not like being treated like a child. Help us where we are weak, but don't give up on us just because we have now been labeled with Alzheimer's.
BUILDING COALITIONS
We need a way to break down many of the silos and build a coalition of companies and sites to work as one. Leaders Engaged on Alzheimer's Disease (LEAD) is a diverse and growing national coalition of member organizations including patient advocacy and voluntary health non-profits, philanthropies and foundations, trade and professional associations, academic research and clinical institutions, and biotechnology and pharmaceutical companies. The only sad part is the Alzheimer's Association National has not joined due to not being able to set politics aside. Another example while it is early in the development is Dementia Friendly America (DFA). It is only this way that we will be able to address the issues. Government or one company cannot do this alone.
http://www.leadcoalition.org/
http://www.dfamerica.org/
This is all part of the problem - a lack of willingness to work together. I am not sure what the state can do here but we need to find a way to encourage others to work in harmony for the greater good of what we all seem to claim. We are doing this for dementia. Sometimes I really wonder and I think it's just a business for these folks.
I know I have made many recommendations around the use of the Alzheimer Association as part of this document. Because of that I want to give full disclosure. I was a past ESAG member and an ambassador for them. For those who know me they would tell you I am not influenced by others and my dedication is to those impacted by the disease. With that being said I do feel they deserve a lot of credit for what they have accomplished in the last 30 or more years. They take a lot of heat for some issues that are out of their control due to some high level expectation of the public.
On the other hand I do not want you to think that they have all the answers because I and many others realize that they do not do justice for many like me who are dealing with the disease. They focus on the caregiver and not us. Part of the problem in my eyes is the lack of a business-mind across the board, and lack of a CEO approach to business. Because of that scenario there is much inconsistency in the organization and much time is lost in understanding our needs and minds. That all leads to very slow response or lack of response to the very services they think are great. They have this internal mindset that everything has to be done a specific way and that is always the right way, yet the people are not given the tools. The sad truth- it is not and I have worked on changing some of that and I can assure you it's not an easy task. I encourage that we continue to work with them but at the same time we need to demand change and at a much faster pace. As I update this version today they are in the process of doing exactly what I had recommended back in 2012. I do believe over time this will benefit all of us. I also think it will be painful along the way. We need to keep the best practices from the chapters that do good and make those programs standard at all chapters. For example my local chapter does not include people with dementia on its board unless they also contribute 10,000 dollars, yet others don't ask for money. I also believe top management should not grow. They should also focus on what is important for the people living with dementia instead of being focused on their financials or do anything controversial. The mission should and must be focused on those impacted by the disease.
------------------------------------------------------------------------------------------------------------------
I am sharing this with you in hope that, as you do your planning, you take my findings in to account when making recommendations to others. We must treat all people who are living with dementia, regardless of stage, with the highest level of respect all the way through to the end. While this may not apply to all, it would appear that many who are even in stage seven are still able to communicate in some way.
ADDITIONAL LETTERS & ARTICLES
RECOMMENDATIONS TO ENHANCE CLINICAL TRIALS
TO: Pharmaceutical Executives
FROM: M. Ellenbogen - Advocate & Person living with young-onset Dementia
RE: RECOMMENDATIONS TO ENHANCE CLINICAL TRIAL ENGAGEMENT
I have always had a different view of things than most people, which led to business success and meaningful contributions to many organizations throughout my life. I know that important issues must be addressed by top-level executives. I appreciated good suggestions from clients and acted on them when I saw the benefits. That is my goal with these recommendations to you. Most can be done with little or no added cost while enhancing participation and accuracy in clinical testing:
Development through Collaboration
Bringing a new drug to market has become very challenging for many reasons that you are aware of. Considering that Dementia, including Alzheimer's is the third leading cause of death in the US your companies need to step up to the plate collaboratively to deal with this national and global societal epidemic.
While I understand you cannot do it alone there is no reason why you cannot partner with others in your arena. Identify ways others have already tested to stop wasted duplication. Concentrate efforts together and share the profits in the end. With the access of technology today we must really change our ways of how we do business. A clear database must be established on all failures. This will be a huge cost saving to all in the world. The price of creating it would pay for itself in no time if all contributed to such a project.
National Registry
A national registry of people living with dementia should be created and shared for all dementia-related clinical trials. This should be a collaborative effort by all companies and entities engaged in clinical trials. Consider incentives to get people to register.
Reposition the Benefit of Clinical Trials
A major problem is getting people into clinical trials. Trials are often described as "the possibility of a cure with no guarantee or access to the drug at a later date". Most caregivers and patients feel that it makes no sense to go into these trials. Most say it is hopeless for the patient and not worth doing.
I believe you need to say that participation today may lead to future benefits for their spouse or other family members that may be impacted by this disease in the future. Everything learned today will lead to success for the future and will be able to help others who may never have to walk in our shoes. Consider how compelling this approach would be to caregivers who are often the influencers or primary decision makers.
Reduce Involvement of and Impact on Caregiver
A major barrier to participation is the added burden on already-overstressed family caregivers who cannot afford to take extra time away from their jobs to accompany their loved one to additional and unnecessary visits for trial sign-up and appointments. Many caregivers are afraid they will be fired or lose pay for taking off so much time; these unspoken fears are a significant invisible barrier to participation!
Don't Diminish the "Personhood" of Potential Participants
An important barrier to participation is the tendency to treat the person living with dementia as incompetent. "We are still capable of doing many things on our own and should be treated with the same respect and dignity given to other adults."
Use Technology for Sign-up Flexibility
New tools like Skype, Zoom should be used to simplify the sign-up process by using a computer or tablet. Create a simple disk that takes care of all the steps to insure the technology is not an issue for the user. I had setup an appointment to volunteer for a program. I received a call that I would not be able to attend if I did not have a caregiver with me. The reason they need the person is so that they can complete a short survey and complete some paper work. All this should be done remotely.
Cost Factor
I believe the cost for participating needs to be covered 100 % as soon as they enroll. Some cannot afford any delay as they are struggling already. The average family is hurting financially due to this disease. People should not lose money because they are trying to do something good. Most likely what they are doing will not help them but the benefits gained could be priceless to others. Keep in mind that they are offering their bodies and being in a clinical trial is very stressful to them and their family.
Changes in Neurological testing
I believe information collected from Neurological testing is flawed because they always use the same words. There should be 3 or 4 different card sets that are alternated throughout the process. You especially do not want to use the standard ones I use with my regular doctor because I have them memorized.
Valid Self-Reporting is a Major Problem
I understand the need to get a list of side effects or issues that may be impacted by your trial. When we come in for a visit, the doctor asks us if there are any issues to report. We are struggling to remember what we ate a few hours ago and they expect us to know what issues accrued. This is not like other clinical trials because it is extremely hard for us to give you accurate information. It may even be wrong information that we believe is true. You need to consider how valid this approach is.
Partner with organizations that do not charge any fees for service
I heard a doctor speak about the NACC program stressing their need for volunteers, so I wanted to help. The program was subsidized by government grants and Pharma. After sending in my records it was determined I would have to pay for a doctor's visit just to get into the program. If this is a government sponsored grant with some of my taxes and others who are no longer able to afford the cost, why do the good people who support these programs have to pay? Especially when one wants to volunteer his time and body to help the program.
Because of these fees, I feel that the results may be skewed because the only people who can participate are the ones who have money, which tends to be high-functioning people. Where this hospital was located has a much higher population of African Americans and Hispanics. I believe they may have a better chance of holding the answer to the cure since they are more likely to get it.
Make it more personal
Since participants are meeting with a doctor, give them feedback on noticeable changes in their condition. We really do want to know where we are in our capabilities. We should not be treated like someone with a number. Make it a bit more personalized; give out a mug or other small gift. Just do a little; it will go a long way.
Provide Comfort & Engagement
Many times one needs to go for testing and stay for hours to be monitored. Provide something meaningful for them to do while they are there; TV, tablets, videos, etc.
Testing schedule
In my case I need to see 3 service providers (eye doctor, MRI and dermatologist) every 3 months; and they are in different locations. If it were up to the office they would schedule all on different days. They should schedule all for the same day so you can go from place to place with time in between appointments. With better coordination and planning that should be able to be done. This needs to be in your request to doctors to follow as part of protocol. There should still be the option to go to only one each time. Need to have flexibility.
Transportation
Many people who have dementia are no longer capable of driving or even taking public transportation to get to these appointments. Contracting with local transportation for participants would be most helpful.
While I know there are limits on your part to talk to me directly, I do welcome that opportunity. Please feel free to reach out to me. As a consumer and patient I believe I have a different viewpoint. I can also appreciate your side from the business world. I don't have a long time so please contact me soo n.
LIVING LIFE WITH ALZHEIMER'S DISEASE
Below are some articles I have written in the past, you may learn how someone with AD is dealing with this disease. These are my favorite that I feel people have been able to learn and see another side that they did not know before.
I have worked on this for about five months, and recently I shared the email below with many sites related to AD for feedback. Most of those who had reached out to me were able to support my findings. The bottom line is that while most of us have limited thinking capacity many are able to communicate; we just have to find a way that suits the individual. I received a lot of feedback. My biggest concern is that most people are clueless, and assume that we cannot understand what they are saying about us; many say cruel things. Just try to imagine for a minute what it would be like to hear what others may say or do to you, and you are never given an opportunity to defend or express yourself. That is what is happening to most of these folks.
We must find a better way to educate caregivers, health professionals, and all those working with people living with this disease. The biggest problem I see is that everything is time-based because of the costs. This view will not work for people. It will also take special training, and the need to break with our normal habits of communicating. If we are going to be able to reach out to them, we need to change. We are still human beings and we deserve to be treated in a respectful and dignified manner.
My name is Michael Ellenbogen and I have been living with AD much longer than most people who have had this devastating disease. I am in need of your help to prove a point. Let me explain.
I have learned that as we progress with Alzheimer's/dementia, we lose our brain functioning and can no longer think. I am starting to believe that this is not true.
It has now happened to me on multiple occasions where I was asked a question, and I am able to formulate the answer in my mind, yet I found myself unable to verbalize it. Sometimes my mouth may move but nothing comes out. It was the weirdest thing, and I could not understand why it was happening to me. I was aware of what was going on, but could do nothing.
Since that time I have asked 18 other people with some type of dementia, and of them 16 had similar experiences. Two of them said they had not. This makes me think that as this disease progresses our brain may still be functioning, yet it is unable to communicate with the rest of the body, allowing it to have less control than it would normally have. I truly believe I am on to something, and was curious as to how I can try to prove this theory.
Let me give you an example. About three years ago I met the daughter of a man with AD. He was no longer communicating with her because, she was sure, he could no longer communicate at all. Someone suggested she ask a question, and keep totally silent for at least two minutes after. About a minute and a half later he finally responded to her question. From that time on she realized what she had to do and was thankful for that advice.
I don't want you to think it's going to be that easy; it will take a lot of work, patience and persistence on your part. Here is what I would like others to try for someone who is in the late stages of Alzheimer's. First of all take the person to a very quiet room; it should not have any kind of background noise even from things like an air-conditioner blowing. Those noises are real problems for me, and would assume it will be a bigger issue for them. Such noises really have an impact on my ability to process and focus. You should also do this at a time of day that they are not tired. It becomes very challenging for us to try to focus and listen to what others say. It really becomes tiring, and we get burned out quickly.
When you start to speak to the person use short sentences, and pause in between them so they have time to process what you are saying. That is very important. Tell them that you think you have found a way to communicate with them. Tell them you are going to look at them closely for some sort of sign. It could be an eye movement, maybe looking to the right or left or down or up. It could be a smile. It could be a finger moving or a fist being made. It may even be them sticking their tongue out. I would start by focusing on parts of the body that may still show signs of control. You must become a detective and keep looking at various body parts for some sign. It may not happen the first time or even a second time. It may never happen and I could be wrong. But if I am right just think of the benefits that will come out of this for you and your loved one.
Reassure them that you will continue to look for a signal and they should keep trying the best they can at their speed. Ask them a simple question like "do you love me? If yes lift your finger or lower your finger". Again you will need to keep quiet, and observe for at least two minutes. Keep doing this and try this with different parts of the body. They may not have control over certain parts, and that may be an issue. If you do see something make sure you point that out to them and ask them to do it again to insure they really are responding. If this turns out to work find a way to use that same body part to get yes or no responses from the person. Keep in mind that this may not always work and you may need to be creative. Maybe just keep the finger raised longer if they mean no, or tap it twice etc., but that may be too much to ask.
Also keep in mind if the person has not had any real dialogue with someone for a long time this would also take more time. No matter what do not become discouraged, try this at least three different times on different days. Like I said this may never work and I have it wrong. If this does work please reply to this site with your contact information so I can speak to you. If this works for a few it makes me believe that we need to treat these folks completely different to the way society treats them today. This will change so much about what people really believe is happening to our minds.
Tips for Visiting by Laura Bowley, Director, Mindset Centre for Living with Dementia
On the heels of a much-publicized plea from Alan Beamer--a gentleman in the USA with Alzheimer's disease--for his friends to visit him, Michael Ellenbogen and six other people with dementia participated in a meeting to discuss barriers to visiting people with dementia. The discussion took place via Zoom video conferencing and was recorded with the participants' permission. A portion of the taped discussion was turned into a short video to let Mr. Beamer that he was not alone, that most people with dementia experience a drop-off in friends, and that the stigma of dementia affected them too.
All participants agreed that friends not visiting is--as one participant said--"epidemic." As an example, Kelly talked about his own brother, who also has Alzheimer's disease. He has been pushed out of a Board he sat on, and the decline that has taken place since has noticeable.
Michael said he could relate to Mr. Beamer's situation and found it heart-breaking. He suggested that society adapt to conversing with people with dementia by not speaking as quickly or by not using long sentences; be conscious of when one is "rambling" when speaking with someone with dementia. People with dementia spend a lot of time processing what is being said, and Michael suggested that the other people involved in the conversation could use short sentences and leave up to a 90-second response time for the person with dementia to digest the information and formulate a response. Michael felt that while it's important to educate people about allowing time for a response, it is equally, if not more important, to educate people with dementia that it's OK to be in these situations where they might not always speak coherently and require extra time, rather than choosing to shy away from conversations.
When asked if it's easy for people to sit through 90-second gaps in conversation, everyone agreed that it's a very difficult thing! We are primed to jump into a conversation and we look for the cue of silence to speak. It's very hard to break this habit.
Michael pointed out that a 90-second gap is a guideline, but someone in the earlier stages may not need as long, while others may need more time as the disease progresses. Michael said that he easily loses his train of thought and gets lost in a conversation if the others do not pause and be silent until he catches up.
The group talked about ways to facilitate a conversation, recognizing the need for gaps.
Susan noted that the topic of conversation during a visit with a person with dementia can be anything that one used to talk about; topics don't necessarily need to change with a diagnosis. For example, Susan said she can still talk about big topics, such as climate change. She continued by saying that
activities help create a common ground and again, can be anything the friends enjoyed previously, including listening to music, playing instruments, going for walks, puzzles, and games adapted to the person with dementia's changing abilities. These activities are appropriate "pretty far into the progression."
Jan talked about being in a group of people and the challenges for a person with dementia of participating in the conversation. If the conversation begins to go on without the person with dementia, as tends to happen, how will the others in the group know when the person with dementia has something to say? One would expect the onus to be on the others in the group to be mindful of the person with dementia, but Jan pointed out that it's also the responsibility of the person with dementia to take the initiative to ask to return to a topic. While this might be difficult for a person whose symptoms include apathy, it's interesting that we need to make room for a person with dementia to take that initiative, to allow that person the freedom to take responsibility by not stigmatizing him or her as someone incapable of taking responsibility, and that a person can feel so stigmatized that they themselves feel incapable of taking that responsibility. As Michael said, part of the problem may be that some people with dementia self-impose limitations; they choose not to go where it's noisy, for example.
Susan noted that there's no "one size fits all" solution for inclusion in a conversation because each relationship is different. She talked about one idea for navigating a conversation where periods of silence are required: a talking stick. Only the person holding the talking stick may speak and a person can give up the talking stick if he or she has nothing to say. But this can only be done with people who are open to using this system. Basically, the person speaking need only give some clue that he or she needs time, but the onus is on that person to express the need and the signal to be given. The talking stick can act as that signal, but our job in society is to make it OK for people to express their needs and to talk about what works. Susan says she doesn't mind silence; one can learn to be silent.
On the opposite spectrum, Michael said that in board meetings he is given permission to interrupt because the others know he would lose his train of thought otherwise.
As a whole, the group admitted to being very aware of forgetting the words for things -- the nouns! Teresa talked about the stress she puts on herself when she goes out and can't remember the correct names for items, so she's better at home where an environment has been created where it doesn't matter if she substitutes the wrong words. But when she is out, she is acutely aware of how others may perceive her if she uses the wrong word. Chuck said that having dementia can affect one's ego--how one thinks he or she is perceived by others. People with dementia don't want to be seen as "the village idiot."
Teresa says that people need to walk in her shoes--to use her brain for an hour--and then people might understand how hard it is and how hard she tries. People with dementia know their limitations and the need to get others to recognize their limitations. As Teresa says, "If I had no arms or legs, you'd see that and you'd know how to help. You can't see my disability, so it's on us to try and let people know how they can help."
As an example, Teresa decided to let a neighbour know that she has dementia She asked the neighbour if the flag on their house was left up all year, as she was planning on using it to orient herself to the location of her own home. She told her neighbour that she has dementia, and since then, if he sees her out walking or on a run, he'll stop his car and roll down the window to check with her that she's OK.
The Realities of Alzheimer's and Overcoming Stigma
Alzheimer's disease and other forms of dementia affect more than 35 million people worldwide today. An astonishing fact that today someone in the world develops dementia every 4 seconds. By the middle of the century more than 115 million people will be affected by the disease, if we do nothing.
My name is Michael Ellenbogen, and I am living with Alzheimer's and trying to make a difference. I was previously a high-level manager in the telecommunication industry. In 2008, I was diagnosed with younger-onset Alzheimer's disease (YOAD) after struggling to get a diagnosis since my first symptoms at age 39. Losing my job and not being able to work had a huge impact on my life as I was a workaholic. I am now an Alzheimer's advocate and a spokesperson for the Alzheimer's Association (U.S.) as a member of its national 2012 Early-Stage Advisory Group.
I am so frustrated, because no one realizes how seriously disabled I am. If I had a loss of limb or some other visual ailment, it would make people realize. I don't want them to feel sorry for me or pity me, just want to be understood. So many people say you do not seem to have Alzheimer's, and that frustrates me. Let me tell you what it's like to live with this debilitating and progressive disease.
Imagine for one minute that your friend, relative or family member has Alzheimer's and has to deal with the following issues. When I go shopping and look at items, most of them never really register in my mind, even though I see it clearly. I have trouble making decisions, because I question whether I am making the right one. I can no longer enjoy my favorite hobbies, because it requires processing skills that I no longer have. I went from being a gadget person, to now being threatened by technology that I no longer can use. This is what I deal with and so much more.
I go to a happy affair only to be tortured by the noise and surrounding conversations, because of the loudness that cannot be filtered out. If people try to speak with me in a public setting where there are many other conversations, I just don't understand what they are saying. This is because all of the people speaking come in at the same volume level. All the words run together, and it sounds like a foreign language.
I went from being extremely proactive to becoming much less active and motivated. I leave things around the house and don't put them away, because I don't know where they go or feel I may not know where to retrieve them again. One moment I am nice and another I may fly off the handle. I can no longer write or speak like I used to. My friends slowly become distant and usually speak to my wife. I do realize this.
I worry every day about the challenges ahead. Or even worse, I am losing my mind and see it happening, but I cannot do anything to change the course. People always say "if I can do anything just let me know." If I take them up on that offer, they back out of their commitments. I have become extremely surprised by the lack of public commitment to my pleas for support of Alzheimer's disease. While some may be sympathetic in the moment, there appears to be little follow-through. This is very upsetting, because I feel as though it affects me personally as well as the millions of others living with the disease. I was always there for others when they needed it and now I feel alone.
While many people just coast through the day, I have to use 110% of my processing skills to do most things, which increases the stress and frustration. The worst part about this disease is knowing that I am doing all these things wrong and have no way to control or stop it, and it's only getting worse as the days go by. I used to save lots of money by doing so many things around the house. Now I lost the drive, determination and skills needed to do those things. Many times I hurt myself trying or make it worse.
I cannot begin to explain how it tears me up inside to see my spouse struggling to do the things that I once was capable of doing and know I cannot do a thing to help. I realize that one day I may no longer be able to drive and this devastates me. I see my wife becoming stressed, depressed and overwhelmed, but caregivers know it will only continue to get worse. Sadly, they keep telling themselves that they can do it all even when we know they will need help.
I, the patient, see it definitely. My wife is on the road to hell, and she does not even realize it yet, because she is so busy trying to block it all out. The worst part about all this is, I have not even reached the worst stage. That scares the hell out of me.
I have been so surprised by the stigma associated with this disease. It comes at you from all angles. People think they know what Alzheimer's is, but they don't. I see this not only from people living with dementia but many media health correspondents, physicians and organizations that are geared to helping those deal with the disease. I have learned that I do not want to share my diagnosis with people I meet until they get to know me. If I was to tell them upfront, I would be treated so differently, which I have learned. I kind of see this disease like HIV used to be. The people who have it are so afraid to let others know, including family. I do not get it. We did nothing wrong to get this disease, and we need to speak up to let our voices be heard. We did nothing wrong and no one should be ashamed of having it. I feel so much better when I share it with others than when I try to hide it.
Because of my frustration with the existing environment for people with dementia, I realized change was need. I decided to use my few skills left to advocate. I have spent some of my last few years being on television, radio, newspapers, many blogs and working with many politicians. I also had an opportunity to speak at all of the public sessions to develop the first U.S. National Alzheimer's Plan, all this on my own. But that was not enough, because I ran into so many people who just did not want to get involved. I was a volunteer for the national Alzheimer's Association Early-Stage Advisory Group. If there is something I want you to walk away with it's that you can make a difference, but it will take persistence. Write a letter to your public official or reach out to local support organizations to create needed programs and services. Your voice and your story are powerful tools. Please get involved.
The simple truth is, if you have not been touched by this devastating and debilitating disease yet, consider yourself extremely lucky. Sadly, it's just a matter of time before it touches you. It is my hope that my actions today may prevent future generations from suffering with this disease. So give yourself piece of mind and do something today. I hope that what I am doing will allow me to leave this world knowing that I did everything possible to make that next generation have a fighting chance. There are no excuses for not wanting to help. The human cost factor is too high, and we are all accountable to do something.
There are many organizations out there like ADI and the Alzheimer's Association that can help you. The Alzheimer's Association got me started in many ways with my new journey. It not only helped me, but it also had helped my wife as my caregiver. They have a website with many resources at http://www.alz.org. I encourage you to reach out today if you have not already. I would also encourage you to educate yourself.
Please join me and Go Purple on Sept. 21 for World Alzheimer's Month. I wear a purple Alzheimer's bracelet every day. And for those living with Alzheimer's, stop focusing on what you cannot do and join me in the battle to advocate. We still have so much to give, and we need to use our skills at our own speed. There is nothing to be ashamed of. We are counting on all of you.
------------------------------------------------------------------------------------------------------------------
Over the past few years I have visited many websites that talk about Alzheimer's/dementia. The one thing that they all have in common is that not one of them encourages those of us who have the disease to continue to live and enjoy our lives. While I realize AD is a progressive and devastating disease we are still here, we are still alive, so treat us that way. Do not write us off.
I have always been savvy when it comes to finances and have always been a saver. One day I was speaking to a friend of mine who has AD, and I was telling her how I did not want to spend a lot of the money I had saved, because I wanted to leave it for my wife for that rainy day. My friend told me: "This is the rainy day. What are you waiting for?" She was right, and that's exactly how I started to think.
Just because we are living with AD, does not mean we should curl up and think our life is over before it actually is. There is so much more we can still do to enjoy life. Make wonderful memories with your loved ones before the days turn ugly.
One thing I had always wanted was to own a convertible, so we purchased one. I wanted to drive it down to the Keys in Florida. I have a friend out in California who also has AD. She has an RV and had planned to travel around the country before she declined and was incapable of driving anymore. One day she mentioned that she was going to the Keys and I decided to meet up with her. I also wanted to go deep-sea fishing to catch a big game fish. Don't get me wrong I am not person who goes fishing, but it was something I have always wanted to do. I had looked into it and it was very pricy, but it has always been on my bucket list. I think we all have a list if we stop and think about it.
I had no real plans; I just wanted to go out and drive my convertible, to feel the fresh air and admire the beautiful scenery and enjoy nice weather. I had a great time. I had a permanent smile on my face. I decided to stay with my friend in the RV for a week and visit various campgrounds along the way. That was a whole new experience, and some of the places we stayed at had fabulous views.
It was great to be out on our own, not having to rely on caregivers all the time. We had some difficulties, but we were able to manage on our own. It cost me a few extra dollars along the way because when I purchased something I could not remember the price in order to be able to compare, and sometimes I took the wrong road and had to take the turnpike, but these were minor issues. This road trip made me feel so much better about me. It was good for my mind; I came back stronger because of what I had achieved.
This disease has a way of making you feel like you are no longer cable of doing things on your own. You lose your self-esteem and your self-confidence. After this trip I felt great.
I did have to opportunity to go fishing. It was such a beautiful day with perfect conditions. The fish were not really biting to begin with but it didn't matter I was just happy to be on a boat again. Then I caught a fish that was about 10-12 inches long. Then I caught a barracuda that was at least 18 inches long, and then one over two feet long. Not to long after that I got the big one, a king macro that was 42 inches long! You should have seen the smile on my face. It is memories like this that we need to be making.
My friend in the RV has decided that she will not just use her mother's china and silverware on special occasions. Instead she took them with her in the RV. It gives her pleasure to use them every day. How many of you have a wonderful expensive hand bag or nice watch, which you only use on a special occasion?
Life is short; take pleasure in using those treasured items now. Start to create your own bucket list, don't just write it, DO IT! There are many wonderful memories that you can still make. Make them now before it's too late. Stop focusing on the negative. Make these last few years be the best of your life. You must do this now, before your mind no longer works.
------------------------------------------------------------------------------------------------------------------
Since being diagnosed with Young Onset Alzheimer's Disease I have dedicated much of my time to its advocacy. Over the years I have worked with many people in different parts of the world, and through my experience I have come to realize that a major problem in reaching a cure is our actions. The way we treat not only those who have this disease but those who care for them, the focus on funding and research and the lack of communication and collective action. Although there are many brilliant people who are involved in Alzheimer's and Dementia action and research I feel that following some simple principals and plans we could bring about real change in the world of these diseases.
PARTICIPATION -- Patients, caregivers, family and friends must become advocates
FUNDING -- Unprecedented action from government and public sector is vital
TEAM WORK -- Organizations dedicated to fighting the cause must work together to reach a shared goal
RESEARCH -- It is imperative that professional medical research personnel work hand-in-hand with patients
LIVE -- Those with the disease must learn to live happy and fulfilling lives
PARTICIPATION -- The government wants to hear from us! I have been doing this a long time and I am told over and over again by government officials that they need to have a clear idea of the numbers of people with Alzheimer's so they can make the appropriate changes to policy etc. In order for the government to do something they need to see people with the disease. I know people have busy lives but if we want things to change, patients, caregivers and friends need to start taking action.
How can you help? By getting involved! Write to the people who can help -- government, health officials, and the press. But be mindful that you have to be persistent with these people, you have to fight. Can you imagine the impact if even a small percentage of the millions of people with dementia took a little time to have their say?
FUNDING -- We must look at other funding models for this disease. Unlike HIV and cancer, there are no survivors. Patients will continue to place a massive financial burden on the national economy; we need to be more proactive in how we fund research, care, medication and support for loved ones and caregivers.
How can you help? By writing to Congress, and the National Institute of Health. These people are responsible for prioritizing the distribution of funds to critical diseases -- Alzheimer's disease is not on the list; we need it on the list.
TEAM WORK -- There are many organizations out there hosting their individual fund raising programs, which is to be commended but the downside to this is that they still insist on operating independently on one another. These people need to see the bigger picture, they need to set aside their politics and differences, and come together as one and work together -- after all, they share the same goal don't they?
How can you help? Well we can stop complaining about these organizations and give them solutions and guidance. Together we have the power to bring about change. Keep informed of all the latest news and action, don't listen to gossip or rumor -- check the facts; do your homework.
------------------------------------------------------------------------------------------------------------------
My name is Michael Ellenbogen. I am living with Alzheimer's disease. I spend almost every waking hour advocating for increased funding for research that will improve the treatment of this dreadful disease. In 2008, at the age of 49, I was diagnosed with Alzheimer's disease after struggling to get a diagnosis since my first symptoms began at age 39. There are more than five million Americans now suffering from this devastating disease.
The National Institutes of Health (NIH) funds research into critical and devastating diseases such as cancer and HIV/Aids. Yet there is much neglect and discrimination regarding the allocation of funds for research into Alzheimer's and related dementias. As a person who experiences the devastating impact of Alzheimer's disease every day I hope that research will lead eventually to postponing the onset or slow the progression of this disease, if not prevention and cure.
Currently, Alzheimer's disease only receives about $450 million for research from NIH, compared to more than $5 billion for cancer and more than $3 billion for HIV/AIDS. I am astonished at the lack of funding dedicated to addressing the number one health epidemic. Historically, leadership from the federal government has helped lower the number of deaths from major diseases such as HIV/AIDS, heart disease, stroke and many types of cancers. This past experience provides hope that increased efforts directed at Alzheimer's disease will be met with similar success.
There are many more Americans living with Alzheimer's than HIV; more funding is desperately needed. If we do not act now this disease has the potential to bankrupt this country. Money allocated today will have an enormous return on investment if it leads to the kind of successes obtained for other diseases.
If you have not yet been touched by this devastating and debilitating disease it's just a matter of time. I hope that my advocacy will help prevent future generations having to suffer my fate and that of many others. You can help by increasing NIH funding for research on Alzheimer's disease and other dementias.
I appeal to members of the House of Representatives, the Senate and the respective appropriations committees: Make the hard choices; increase funding for Alzheimer's disease. Do everything necessary to ensure that Alzheimer's disease gets the exposure, commitment and funding necessary to change the course of the disease before millions more Americans are affected.
My work as an advocate has provided opportunities to share my story on a national platform. I have provided public comment during meetings of the Advisory Council on Alzheimer's Research, Care and Services in addition to having my personal essay about overcoming the stigma of the disease featured in the Alzheimer's disease World Report 2012. I have also become a member of the Alzheimer's Association National Early-Stage Advisory Group, helping to raise awareness of the disease and provide insights on the most appropriate programs and services for individuals in the early stage of Alzheimer's and other dementias.
I hope that what I am doing now will allow me to leave this world knowing that I have done everything possible to make generations to come have a fighting chance. Do not forget these people or the future generations who will develop this disease. We face dying in the worst possible way.
As an Alzheimer's patient, I find it very difficult to perform tasks that I was once very capable of performing. Sometimes I am better than other times at doing the same task. People around me have accepted this fact and have tried to be very forgiving when I run into issues doing a task or when just trying to remember something. I really think that people around me should challenge me more at times.
For example, many of my doctors kept questioning me about whether or not I should still be driving. This of course was mentioned to my wife who also started wondering. I finally had a driving test a few years later. It was recommended that I no longer drive, even though I passed the test. I was almost borderline, but there was concern that I may not recognize when I become worse and could then become a danger. First of all, I have to tell you that the test they performed was not fair. I wonder how many regular people would be able to pass this test. The test also relied on me to learn new things in order to take the test. That is not fair since I have been driving the same vehicle all this time and nothing has changed. This constant talk about my driving has totally killed all of my self-esteem about driving. Every time I was in the car on the road with my wife, she constantly pointed out any mistakes I made, and her reaction time was much quicker than mine. I do realize I am a bit slower in my response time, but that is why I give myself more space between the other cars. Sometimes I am very far back or I just don't want to go around that slow car. There is nothing wrong with not feeling comfortable to go around that person. Let me do it at my speed.
I see many people on the road that I feel are so much worse than me and I wonder why they are still on the road, if I am supposedly so bad. I decided that I was going to drive to visit my daughter in South Carolina. I live in Jamison, PA in Bucks County. I was very scared to take this trip but I was trying to prove something to myself. It could have meant the end of my driving if I made a serious mistake along the way. I drove in one day, about 700 miles, with the help of a GPS in my car. The more I drove, the more I was starting to feel comfortable behind the wheel. A few other people on the road made serious mistakes along the way and I easily avoided a possible accident. This trip was the best thing I could have done for myself. I now have almost all of my self-confidence back and my wife no longer makes constant comments about my driving, unless I have a real issue. I have now had two close calls that required quick thinking and maneuvering to avoid an accident. In both cases, I was able to avoid the issues without my wife's comments. Again it may have taken me an extra second or two to react, but I was fine.
WHO'S THE THIEF
Who's the thief? Is there a thief? Why do we say that?
I have read so many stories about people living with dementia accusing their assistant -- I don't like the term caregiver -- of stealing their belongings. As a person with dementia I was hoping I would never become one of those people because I knew it could be very hurtful to those around me. However, as I continue to decline into this black hole that is Alzheimer's disease, I find myself trying to analyze these things to see if there is any truth to them or whether it is simply a misunderstanding. I am an ideal person to look at this issue as not only am I living with dementia but I am still able to share my thoughts on what may or may not be happening.
In the past year or so I have become very accusatory of my assistant/wife when I have not been able to locate something. In my mind I know I had put something in a certain location and it was no longer there. Most of the time it turned out that I was right and my wife had moved it somewhere else, so only she could locate it. I have also been told that I over react and am too quick to blame. That may be true; however, I am not sure why I cannot hold back those emotions and have more control. But the fact is I don't and it is not going to get better, it is more likely get worse as I see myself transforming into something I don't want to become.
Today I woke up and we had snow, so I needed to clear the driveway and footpath. When I went to the place where I keep my boots they were not there. As I searched in various places I kept saying to my wife that she had done something with them. She was helping me look and telling me she had not moved them. I just could not believe that I was unable to locate them. Then I seemed to remember that they may have had some cracks in them.
Although neither my wife nor I was able to find them I was not thinking that someone stole them, even though we'd had had many workers in the house in the last year and these are really great boots. Then all of a sudden I remembered that the manufacturer had sent me another pair. This made it more interesting because now I could not find TWO pairs of boots that are about 18 inches high and therefore not easy to misplace.
My wife kept insisting that she did not know where they were, and now I am beginning to think that they could have possibly been stolen especially since one pair had never been worn. But then I was thinking that maybe I threw one pair out and I am only looking for the new pair. This went on for a while as we both continued to search the house, which in itself has become a disaster zone from the way all of my items have been moved around. I finally convinced myself that they were stolen as there seemed no other explanation and I was not even sure how many pairs we were looking for.
I decided to give up and accept that they were gone and put on another pair of work boots that, although not designed for snow, would do the job. My wife continued to search all of her locations only to come up empty. Then she had an idea and went upstairs and promptly came down with two pair of boots, telling me that if I had put them away in the first place she would not have had to find a place for them. The mystery of the missing boots was over.
Although I was glad they hadn't been stolen, it was much easier to accept them as being stolen so I could justify why I was unable to find them. However, in my mind I blamed my wife since she was ultimately the reason I couldn't find them.
This disease really sucks in so many ways. I don't have a clear vision in my mind of things, just minute spots of memories. And I do mean a spots. I need to be able to magnify the spot in order to make sense of it but I am no longer able to do that. I no longer have groups of thoughts that I can make sense of, instead I have flashes of memories, which may be completely irrelevant to what is going on at that moment.
The only way I can describe it is the way a film works. To make a complete film you need hundreds of still shots per second to build up the picture on screen. Every once in a while I may have one still shot that lacks clarity and meaning before having it fade to nothing in a matter of seconds. So before you think the person with dementia is going crazy you should probably ask yourself if you or someone else moved it or got rid of it. There is something positive to be taken from a situation such as this: at least the person with dementia is still capable of thought; no matter how fragmented.
COPING STRATEGIES FOR DAILY CHALLENGES
Because of this situation, I feel even stronger than ever that it is important to be challenged. I know it may be easier for you to do something for an Alzheimer's patient because it's much quicker for you to accomplish the task. But I really believe that if you take the time to coach us along the way, we may do better in the long run. Believe me, I know it's got to be very aggravating at times, but I really appreciate it. It takes a lot of patience on the part of the helper. Everyone is different and you need to know at what point in time you should not push. It's also hard to be patient and not raise your voice at the person you are trying to help, because it will only make it worse.
------------------------------------------------------------------------------------------------------------------
Daily Challenge: I have trouble remembering dates or things I need to do.
Coping Strategy: I use my computer and Microsoft Outlook to keep me straight by sending me reminders.
-------------------------------------------------
Daily Challenge: Getting email using regular places like Google or Yahoo is a challenge for me.
Coping Strategy: My daughter had set up my Outlook to retrieve emails from all my accounts, and they arrive in the same format which makes it so much easier to read, and it allows me to use common folders.
-------------------------------------------------
Daily Challenge: I forget to reply back to people's emails.
Coping Strategy: I flag them with a reminder date so it will automatically send me a reminder.
-------------------------------------------------
Daily Challenge: Remembering passwords is a real challenge for me.
Coping Strategy: I have created a personal system that works great, I also rely on the computer to store many of them; however, it is a real challenge when the system does not work. I also keep files with the password information.
-------------------------------------------------
Daily Challenge: I have trouble remembering the day, the month and the year.
Coping Strategy: I have a watch that displays all the information.
-------------------------------------------------
Daily Challenge: I have an extremely complex TV, stereo and entertainment system, which requires many remotes and settings to be used.
Coping Strategy: I purchased a smart remote that allows me to put in all the steps at once, and press one button which takes care of sending all the commands to all the devices at once. It works great until it fails. Not sure how much longer I can maintain it. It's a bit involved
-------------------------------------------------
Daily Challenge: Most of my lawn power tools are a struggle to use.
Coping Strategy: I do not think I have any coping method other then I keep trying different things until I get them to work. The problem is most are new, I find it easier to work with tools I am familiar with.
-------------------------------------------------
Daily Challenge: When I drive I don't always feel as comfortable behind the wheel.
Coping Strategy: I sometimes need to take more precautions, and allow more distance between the car in front of me, and I may drive a little slower. I am also much more alert and focused during these times. It makes it hard because when I travel with my wife she wonders why all of sudden I drive slower, when normally I am flying. There is nothing wrong with going slower and being cautious.
-------------------------------------------------
Daily Challenge: I don't do much of anything anymore.
Coping Strategy: The other day I was speaking with my neighbor who was waxing his car. This gave me some inspiration to want to do it. When people mention things to me it sometimes gives me what I need to take it to the next level.
-------------------------------------------------
Daily Challenge: I purchased a camera; however, no matter how many times I read the manual I still don't seem to be able to understand how to use it.
Coping Strategy: Make sure you buy one that works completely automatic without needing to do anything. It is frustrating at times when you would like to do something on your own but just can't remember on how to do it. I have learned to accept it but I still try and fail.
-------------------------------------------------
Daily Challenge: Spelling and forming sentences has become a real challenge.
Coping Strategy: I take advantage of using the computer to guide me in the correct spelling of a word. That is becoming harder because often it cannot figure out what I am trying to say. I also ask others to look things over for me, and to correct them for me. It's kind of frustrating for me because I am really concerned that I may not be able to do this much longer. I have seen a big decline in this over the years. I seem to notice this more than my other skills because I do it so often. While I am sometimes ashamed of sharing it with others, I still need to communicate so I try to not think about it.
-------------------------------------------------
Daily Challenge: Sometimes when I want to do certain things I need to stop and think.
Coping Strategy: If I want to work on a project I will spend a lot of extra time trying to think of the best approach, this doesn't always help, but I tend to work at a slightly slower pace and am aware that things will go wrong.
-------------------------------------------------
Daily Challenge: Finding past emails or letters
Coping Strategy: The computer is such a wonderful tool in so many ways. It allows me to search the entire computer as long as I can remember a word or two in the document I am looking for. While it may take a while I would not be able to survive without it.
-------------------------------------------------
Daily Challenge: I can no longer do many things
Coping Strategy: I rely on my wife for many things nowadays. I am not sure if that is a coping strategy. When anything important needs to be considered, I ask her for her help. She does all the financials, and planning of most things. It is frustrating but I realize I cannot do it on my own.
-------------------------------------------------
Daily Challenge: I get lost or cannot figure out how to get from one place to another. Maps are not easy to follow anymore even the ones that you print out from Google.
Coping Strategy: GPS! I cannot imagine what it was like for people like me before GPS and the computer.
-------------------------------------------------
Daily Challenge: I fear that one day I will be lost or not be able to communicate with others due to a temporary stress or decline in my mental capacity.
Coping Strategy: I have chosen to not be concerned about that. I have a medical tag on me all the time that has my medical condition along with important contact information. I will continue to go wherever I want to go. I realize I will need to rely on others to get there. I will need to ask others for help frequently, and to ask multiple times so others don't send me down the wrong path. It will take me longer to get there, but I cannot let that stop me. Living in fear is also no way to live. I know there are good people that will help me when the time comes.
-------------------------------------------------
Daily Challenge : Some things I do get me very frustrated
Coping Strategy: I no longer try to do those things so I do not get frustrated
-------------------------------------------------
Daily Challenge: I write notes as reminders
Coping Strategy: I only write a few notes as if I have too many they just become overwhelming, and I would lose track of them because there are too many.
-------------------------------------------------
Daily Challenge : I need more time to do things
Coping Strategy: I leave much earlier for meetings and places so I can allow for issues along the way.
-------------------------------------------------
Daily Challenge: If I start to get frustrated doing something.
Coping Strategy: I move on to something else and then I try to come back and do it later.
-------------------------------------------------
Daily Challenge: I fear I may get lost when I go to new and far places.
Coping Strategy: I take a cell phone with me.
-------------------------------------------------
Daily Challenge: When I go shopping and lose track of the person I am with I sometimes start to worry a little bit.
Coping Strategy: I try to calm myself down and look for them. If I cannot find them I will try to stay by the door we came in so I can see them at that register
-------------------------------------------------
Daily Challenge: I had trouble remembering which way to turn off the water in the garage for the hose.
Coping Strategy: My wife added masking tape with a marking pointing to off. No more issues. I have the feeling that over time I will need many reminders like this.
-------------------------------------------------
Daily Challenge: I have trouble hearing people speak in loud places.
Coping Strategy: I try to not go to restaurants or other places where I will be put in that situation if I can help it.
-------------------------------------------------
Daily Challenge: I can no longer use my video recorder.
Coping Strategy: I now have TiVo which makes it so much easier to do things. I still need some help, and my wife can help when I need it.
-------------------------------------------------
Daily Challenge: I try to communicate with much smarter people.
Coping Strategy: I believe that my reaching out to and working with people who are very smart will delay the deterioration process.
-------------------------------------------------
Daily Challenge: When I cut the grass, or do something that requires me to be a bit more stable on my feet.
Coping Strategy: I use a good pair of shoes, or even a low cut boot. It really helps me become more stable on my feet.
-------------------------------------------------
Daily Challenge: I could get hurt while doing yard work.
Coping Strategy: I do not wear lose clothes or short sleeved clothes when doing yard work so I do not get hurt. Wearing shorts has already led to a broken foot because the pants leg got caught on the shifter. I also wear safety glasses. The problem I have is I don't always remember to take these precautions, or sometimes I think it's not necessary because I feel I will be careful if I am doing something that will just take a few minutes.
-------------------------------------------------
Daily Challenge: Just the other day I was thinking in my head that I had to turn a grate on my fireplace, and I was thinking it may be hot.
Coping Strategy: Instead of being careful and just putting one finger closely to feel for heat, I just tried to touch it with three fingers to lift -- I got burned. How do you get a coping strategy for becoming stupid? It seems that my mind is not communicating with the rest of my body.
-------------------------------------------------------------------------------------------------------------------------------------
ADDITIONAL COPING STRATEGIES:
All the people around me know I have AD, so most of them are keeping an extra eye out on me which is nice to know.
I try to keep some type of a schedule. I get up every day at the same time and try to eat at the same time. This kind of helps to do things like taking my drugs or other things. The second I change my routine you can be sure I will forget to take my drugs or do something else.
I double and triple check myself on many things I do.
I try to find some humor in my issues.
I ask people for help and ask a lot more questions of others
I take lots of breaks
I try to know my limits and will not start a task if I feel I cannot do it. Or I will have someone work with me.
A few months ago one of my friends mentioned that I am always talking about things related to Alzheimer's. While I know I spend my days advocating for this disease I did not realize I was that bad. Especially with those I am not trying to convince or influence. Although I appreciate the person telling me, it has really bothered me.
I started to give it some thought and tried to understand why and what I could do to change that. Not too long after that my wife made a similar comment, and that really hit home because their comments to me were so close together.
I realized many things have contributed to this. The most important is I no longer work and I feel like I am locked in this house; I really have nothing else to do. I wish I could still be working and doing something meaningful, but unfortunately my skills required to perform those jobs are no longer there because of my Alzheimer's. I use to go to work, I used to talk with others about many different topics, not just work but everyday world issues.
I have tried to have similar conversations with people about issues in the news, and I don't always have the right information since I don't always understand it all, and only retain bits and pieces. While there was a time I was a news junkie, now I can rarely recall many of the topics or even can tie other stories together in my mind so I can speak intelligently. I have recently found myself starting discussions that go south because I start out with part of a subject, and when we delved into it deeper I was at loss for information. I felt stupid because I could no longer speak about something I once found very easy. I used to be great about talking about political issues which really requires you to know what you are talking about, but now I can barely defend my position, and I do worse for even bringing the subject up, and then I feel bad because I was not able to point out the real issues so the person could really make a true assessment.
Since I have no real job I have made it my mission to advocate for Alzheimer/dementia. I try to keep my mind as engaged as possible. I also try to focus on things that most don't, like the high hanging fruit which is probably not the best for some on like me. That involves dealing with many high-level people. While I do good at first I don't always have the answers they require, and sometimes may come across as not knowing what I am doing. It is very frustrating knowing that in my brain I have the answers, but I just do not know how to retrieve the information needed to help me do what I need to do. Especially when I need it the most, I may remember later on sometimes, but it's too late. There was a time that I could retrieve everything to my favor and keep track of everything one person would say to me.
Then I finally realized I listen to the weather report multiple times a day and I never seem to know what the weather is supposed to be like, which I always used to know. I just do not seem to retain it.
I used to like reading the paper and I no longer do that because I have trouble retaining what I read or I don't remember how the story relates to something I read a few paragraphs back in the same article.
I used to have hobbies that I can no longer do because of the disease. I used to love boating and tinkering with electronics. I can no longer do any of these things. I rarely do anything around the house because I am afraid I will make it worse.
When I have conversations with others I do not always remember what we have spoken about in the past. I always hated it when you spoke to certain people and they keep repeating the same information you had spoken about in the past. I do not want to become one of them. There are so many discussions I want to have but I just can't because the lack of my ability and more. I miss that so much. To have an intelligent conversation with someone that can reply with meaningful information, where we both walked away with some new and interesting facts would be wonderful.
I was never one to blow my own horn, but I do that today so others can see some of the steps I have made in hopes that they feel they are willing to take risks and help me expand my mission.
I have accomplished some great things and I think that is what I may share with my friends. Maybe I am repeating myself and I don't know it. I keep trying to figure out how I can change, but I struggle because I do not know what to do. It seems that Alzheimer's has taken over my life and not sure what or how to change.
-------------------------------------------------------------------------------------------------------------------------------------
American Society for Bioethics and Humanities Speech 10.22.15
My name is Michael Ellenbogen. I am living with Young Onset Alzheimer's Disease. My first symptoms came at age 39. I was not given the diagnosis until I was 49. I'm now 57. What I have to say applies to many dementia patients--especially younger ones who may live longer.
This is a very devastating disease. Until I got this diagnosis, I wanted to live as long as possible, like almost everyone else. Now my goal is different.
I still want to live life to the fullest, but only until it is my last opportunity to control when I die. The reason is that Alzheimer's will take away my ability to control my destiny. Alzheimer's will take away my ability to remember and my ability to carry out my plan. If my plan fails, I will be forced to have a prolonged dying because others either cannot or will not allow us to die, when we would want.
So I do NOT want a prolonged dying after I reach the stage of Advanced Dementia. Here's why:
I have several illnesses that cause me pain: gastric reflux, stomach pain, and stiffness at night. When I reach Advanced Dementia, I won't be able to ask for help or for pain meds, or to fluff my pillow to get comfortable so I can enjoy life or sleep. Instead, I will feel tortured.
Dr. Terman's term, "Dementia Fear" is not just a theoretical fear. It's a real issue. I can imagine myself lying there, uncomfortable all night long. Also, my pain gets worse when I have nothing to distract me.
It is important to me to be remembered for the person I was--NOT the person I am becoming. When my daughter was interviewed on FOX, she said, "My father was always so sure of himself. He's not anymore." That really hit me hard. My current condition is so far from what it was, and it will only get worse. I really enjoyed being a high level manager and being an important part of what was going on, being creative, being a resource for others and giving people advice ...so very different from who I am now.
Furthermore, I worked hard to have an enjoyable retirement. But if I lasted to the bitter end of Advanced Dementia, all the money I have saved would be spent on me, leaving nothing for my wife. That would not buy me anything I really wanted. It would just be time without quality of life. And it would not be fair to my wife.
I used to maneuver a boat with great skill, to navigate close calls, but now I can't enjoy this hobby anymore. I used to enjoy electronics as a hobby. Now if I touch anything, it falls apart. I might even electrocute myself.
I wake up every morning and have to remind myself that someday I will need to end my life. Whenever I decide, it will probably be too soon. But I worry that I will forget to actually do it while I still can, or if I do remember...by then, I may not be capable of carrying it out.
How will I know when "my last opportunity" will come? I won't, for sure. That's why I am certain that I will be ending my life too early. Or if my attempt to hasten my death fails, it might put me in a condition that is much worse. So I just hope my timing is not MUCH too early. And I hope it works smoothly.
I know a Young Onset Alzheimer's Disease patient whose friend promised to give him enough Oxycontin to kill himself. But then the friend changed his mind because he did not want to be responsible for the Alzheimer's patient dying. I can understand that, but now what are his options?
I am afraid of ordering drugs over the Internet. They could be FAKES or just make me sick and feel worse but not kill me. There are so many scammers these days. You can't trust... Who knows what hell could happen if I were to try this way.
I had a friend named Dena, another person living with Young Onset dementia. Probably Lewy Body disease. She took her own life. While I don't know what I don't know, when she first told me about her intent to die, a few months before she did it--I was really upset. I thought her dementia was not much worse than mine. Now I still wonder if she died too early, much earlier than she had to.
I know several people who are still doing reasonably well, but who now store in their home several tanks of Helium that could bring about their death.
As I get to know man Young Onset Alzheimer's patients, I would estimate half or more think about wanting to die while they still can, because they don't want to die slowly in Advanced Dementia. While this of course is NOT a valid survey, what I've found is this: The harder I try to get people to talk, the more they reveal their fear and share their wish for a plan they could trust.
One Alzheimer's patient I know died by inhaling car fumes in his closed garage. He taped a message to the steering wheel of his car. It said, "Sorry I had to do this now, but I was afraid to wait because I might forget that this is what I want to do."
We may never know how many people, like the man who left the note on the steering wheel, who feared not being able to wait longer, will have taken their lives when they would have waited if they had another choice that they could count on.
While Dr. Stan Terman has a very good system to die somewhat earlier--to stop being fed and given liquid... and while it's probably the best out there...it is still not good enough. The problem is that 20 percent or more of us will still be able to stick food in our mouths--even after we have lost much of our other abilities and we meet most of our criteria for Advanced Dementia.
To possibly move up the time, Dr. Stan Terman asked me to try thickened nourishment. I never would have tried it, if he hadn't recommended it. So I experimented with "Thick and Easy." Doctors prescribe this product to prevent choking on food and drinks so they don't go down the wrong way since the next thing that can happen is pneumonia. But have you ever tasted it? It's horrible.even when mixed with my favorite drink. Don't ever give me that stuff.even if my life depends on it. I'd rather die by dehydration. By the way, I added this statement to my Living Will.
Along these lines, I hope physicians and others get this message: Stop thinking of what can make me live longer when I reach Advanced Dementia. Instead, follow what I say now about what I really want. Listen to me. Remember what I ask for and let me die with dignity. Please!
I am revealing myself, my diagnosis, my wishes, and I am pleading with you: Please take action to change our laws. It may surprise you but a NEW law that will let us die when we want, will save our lives. We'll live longer. It will also lower our fears so we can spend the last few years of good living without this awful worry, that our last wishes will not be carried out.
I know many patients whose wishes were NOT followed because of incompetence or unwillingness on the part of their doctors. That absolutely must change so we can have confidence... otherwise some of us will kill ourselves when we can. The laws and Doctor's beliefs should not get in the way of what's so important to us.
Many right-to-die organizations have their own ideas on how one should die. And they do not get along with other similar organizations. To them I say: It is not about you or what your organization stands for. It's about the patients you say your organization is trying to help. Break down your silos. Figure out ways to work together to reach a better solution for this horrible problem and this devastating disease.
Thank you.
|









































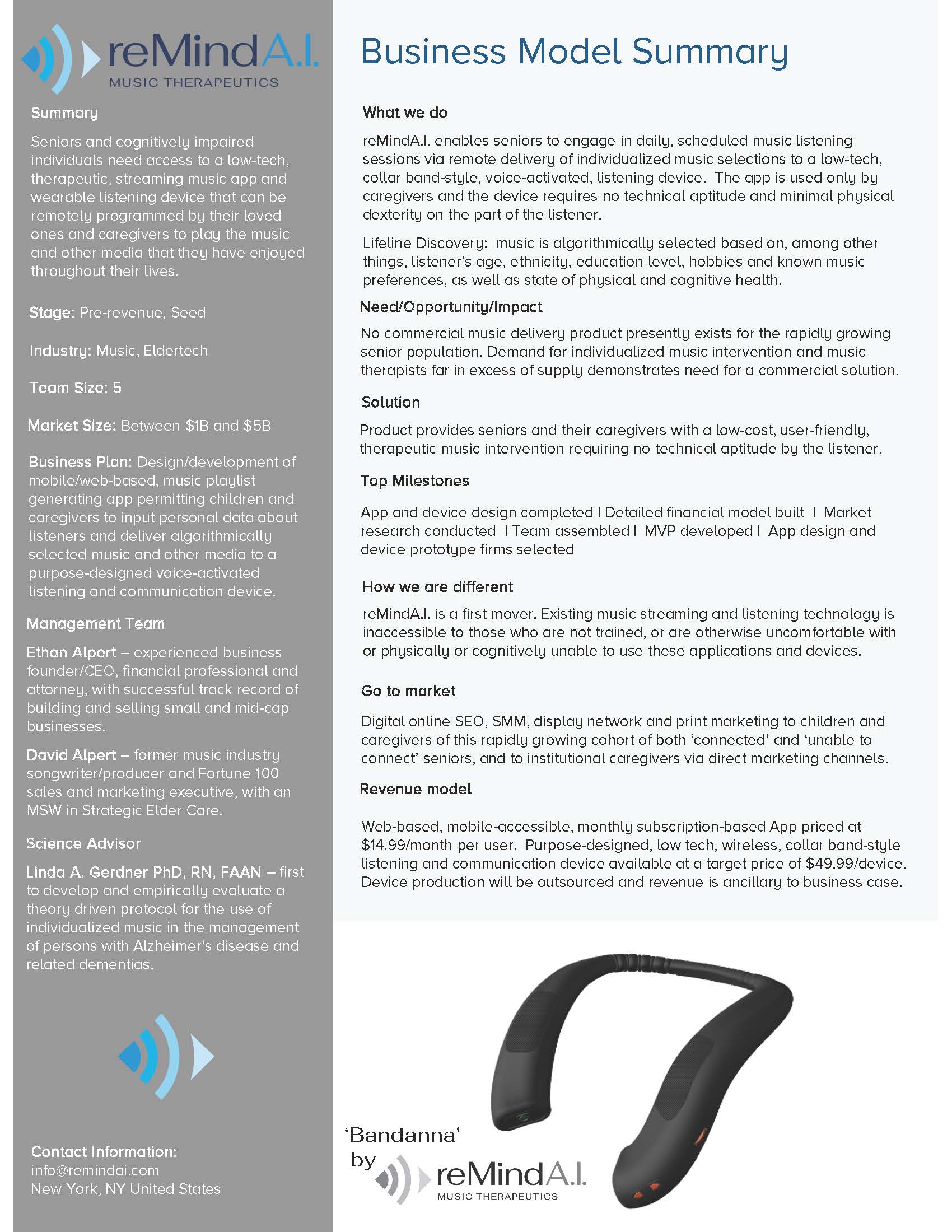
 basic research to market = 16 years)
basic research to market = 16 years)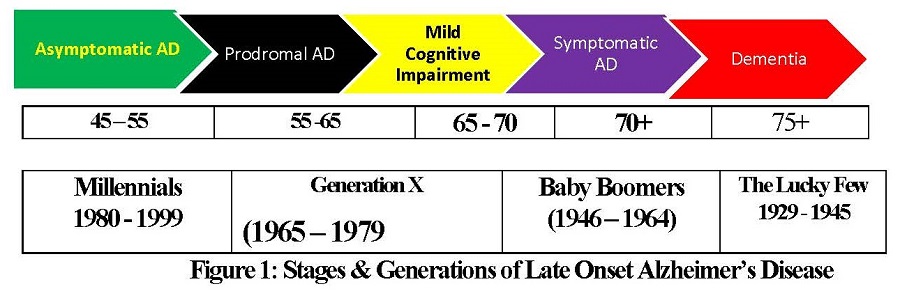
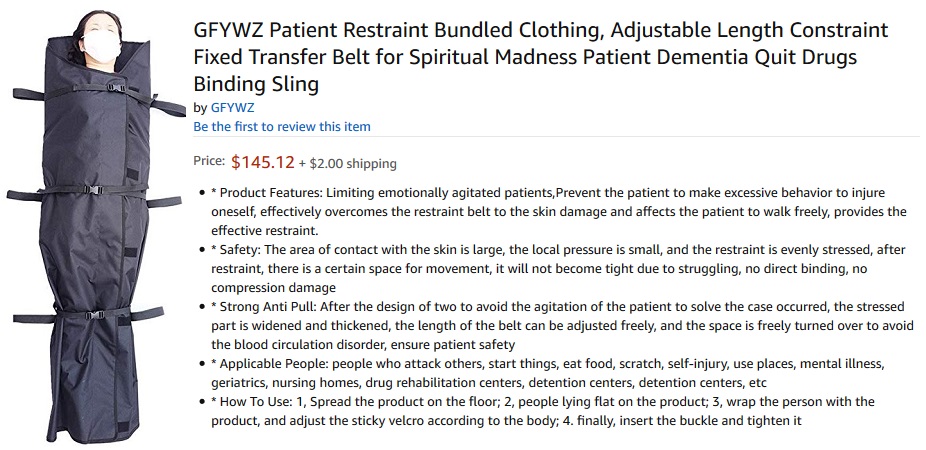
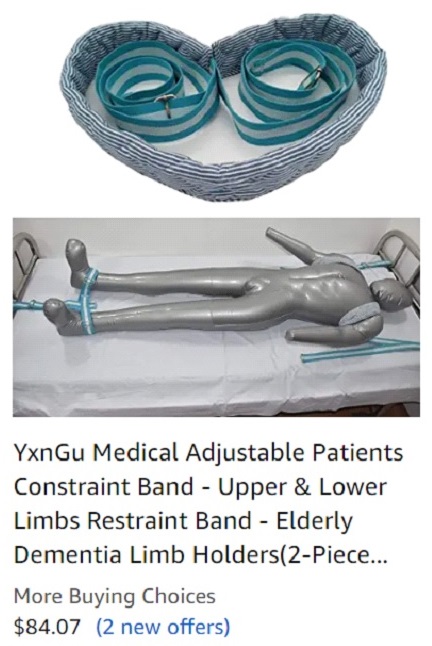

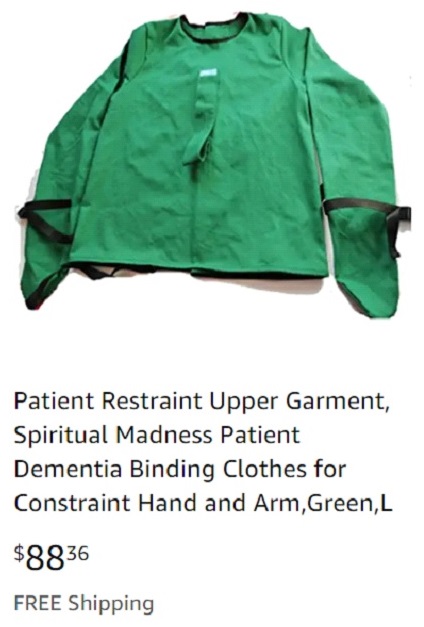
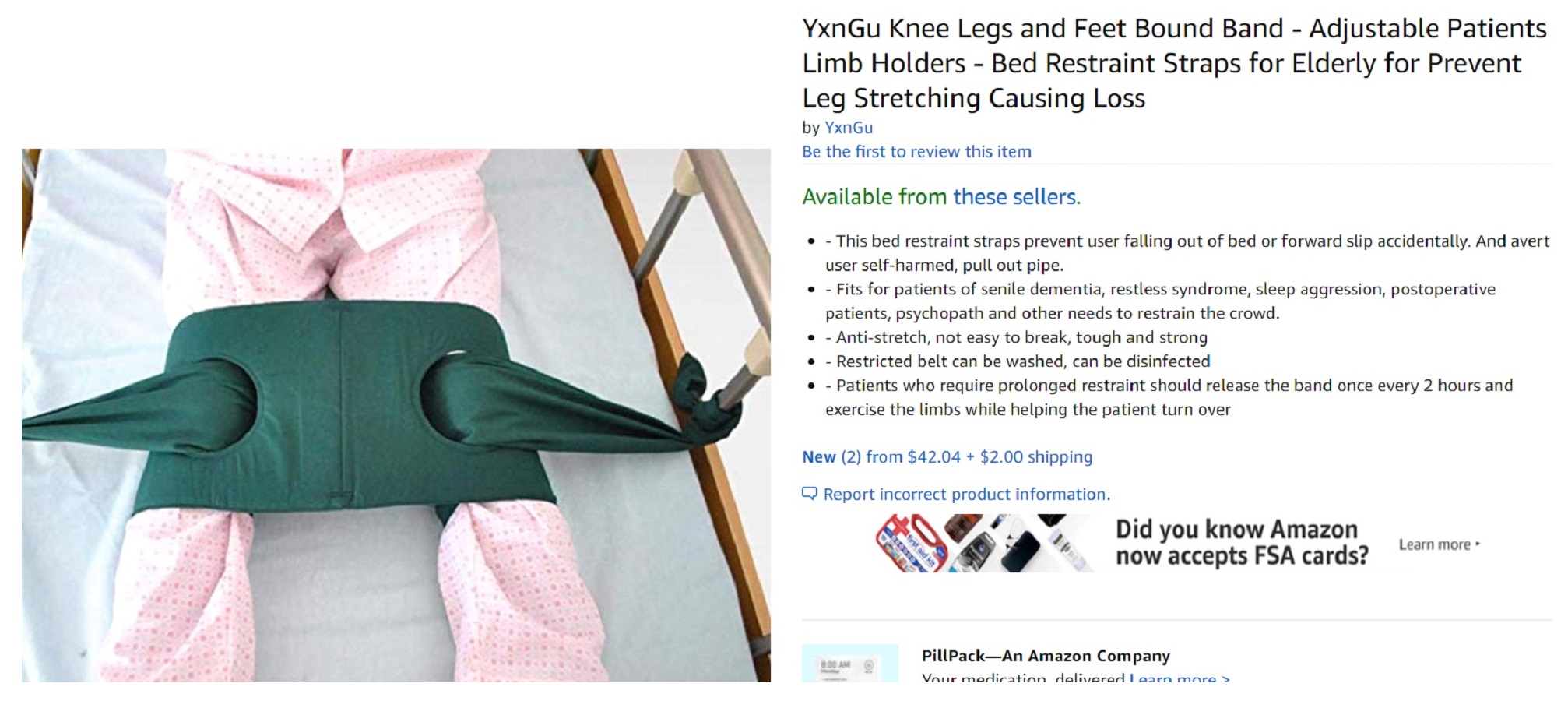





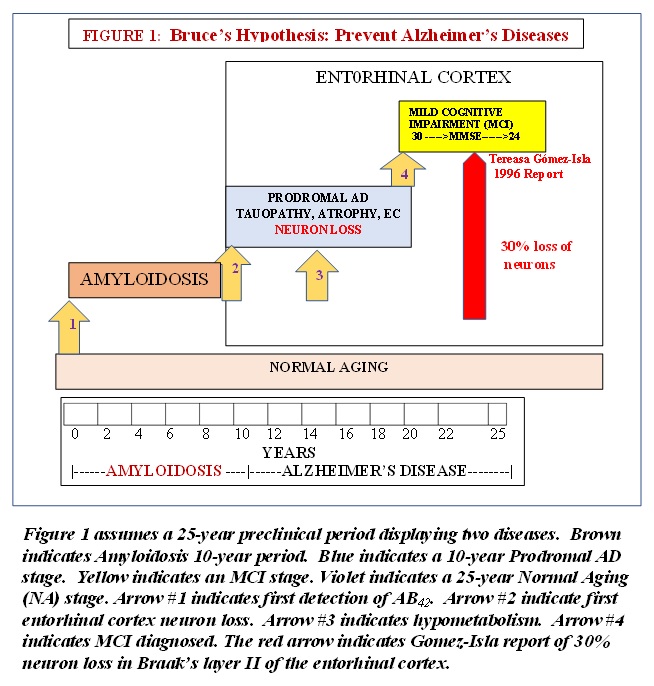









 To be used on all websites and dementia patients information and hospitals
To be used on all websites and dementia patients information and hospitals For stores and businesses to show they know and have been educated
For stores and businesses to show they know and have been educated

 To be used on all websites and dementia patients information and hospitals
To be used on all websites and dementia patients information and hospitals For stores and businesses to show they know and have been educated
For stores and businesses to show they know and have been educated