Westat
Printer Friendly Version in PDF Format (3 PDF pages)
ABSTRACT
As the opioid epidemic has evolved into a national crisis, the need for treatment has increased greatly. Medication-assisted treatment (MAT) is a “whole-patient” approach to the treatment of opioid use disorder (OUD) that combines the use of medications and psychosocial supports, such as therapy, counseling, self-help groups, and case management. MAT effectively treats OUD by decreasing opioid use and opioid-related overdose deaths.
This study aimed to describe different models of psychosocial supports in MAT for OUD. Specifically, the study examined current practices of psychosocial support and factors that facilitate or hinder these models in clinical practice. An environmental scan was conducted that included three components: a literature review, analysis of unpublished survey data, and key informant interviews. In addition, one-day site visits were held at five different treatment programs to learn how organizations implement psychosocial supports in their MAT programs.
This brief was prepared under contract #HHSP233201600025I between HHS’s ASPE/DALTCP and Westat. For additional information about this subject, you can visit the DALTCP home page at http://aspe.hhs.gov/office-disability-aging-and-long-term-care-policy-daltcp or contact the ASPE Project Officer, Joel Dubenitz, at HHS/ASPE/DALTCP, Room 424E, H.H. Humphrey Building, 200 Independence Avenue, S.W., Washington, D.C. 20201. His e-mail address is: Joel.Dubenitz@hhs.gov
DISCLAIMER: The opinions and views expressed in this report are those of the authors. They do not reflect the views of the Department of Health and Human Services, the contractor or any other funding organization. This report was completed and submitted in December 2018.
INTRODUCTION
As the opioid epidemic has evolved into a national crisis, the need for treatment has increased greatly. Medication-assisted treatment (MAT) is a whole-patient approach to the treatment of opioid use disorder (OUD) that combines the use of medications and psychosocial supports, such as therapy, counseling, self-help groups, and case management. MAT effectively treats OUD by decreasing opioid use and opioid-related overdose deaths.
This study aimed to describe different models of psychosocial supports in MAT for OUD. Specifically, the study examined current practices of psychosocial support and factors that facilitate or hinder these models in clinical practice. An environmental scan was conducted that included three components: a literature review, analysis of unpublished survey data, and key informant interviews. In addition, one-day site visits were held at five different treatment programs to learn how organizations implement psychosocial supports in their MAT programs.
VALUE OF PSYCHOSOCIAL SUPPORTS IN MAT
The available literature on the value of psychosocial supports in MAT is limited. Research findings are mixed, though recent systematic reviews have been supportive of the value of psychosocial supports. In general, the literature is inadequate to draw conclusions about the types or levels of psychosocial services that should be provided, or how to adapt psychosocial supports across settings or patient groups. Yet, professionals in the field, including professional organizations, key informants interviewed, and staff in the visited sites all strongly agreed there is great value in psychosocial supports.
CURRENT PRACTICES OF PSYCHOSOCIAL SUPPORTS IN MAT
The findings of this study demonstrate great diversity in approaches to delivering psychosocial supports. Programs employ a range of psychosocial supports that vary in content and intensity, including individual counseling, group counseling, self-help groups, case management, peer recovery specialists, medication management, and skills learning groups. While manualized evidence-based practices (EBPs) are frequently evaluated in research, in practice, providers use EBPs less frequently or in an unstructured manner.
| A national survey of 1,174 buprenorphine providers on the package of treatment services delivered to their patients and found that: | ||
|---|---|---|
 | 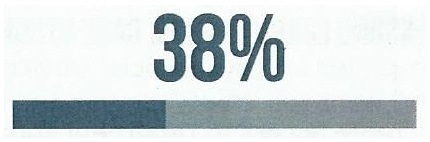 | 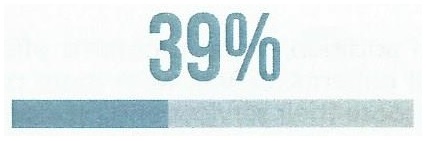 |
| of patients received counseling from the prescriber | of patients received counseling from other providers within the organization | of patients received counseling from external providers via referral |
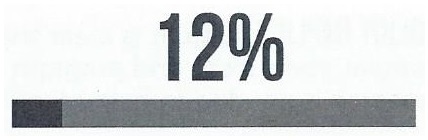 | 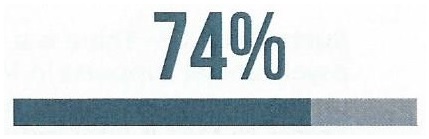 | 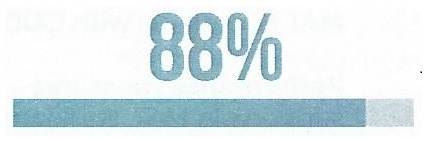 |
| of patients received no counseling | of prescribers increased the frequency of visits when patients continued to use opioids | of prescribers referred buprenorphine patients to local self-help groups |
KEY ELEMENTS OF AN IDEAL MODEL
-
Chronic disease approach: Addiction should be treated as a chronic disease that must be managed over time with the recognition that relapse is common.
-
Patient-centered and flexible care: People with OUD often present with differing needs and levels of severity, so it is important to adapt treatment methods to the individual patient's needs.
-
Stepped-care or phased approach: Psychosocial services should be tailored to the patient's stage of treatment, recognizing there are different goals in each phase of care.
-
Recovery supports: An ideal model of care embraces a "whole-person" approach that includes recovery supports and addresses social determinants.
| BARRIERS TO PSYCHOSOCIAL SUPPORTS IN MAT | ||||
|---|---|---|---|---|
 |  |  |  |  |
| Need for integrated medical and behavioral health care Inadequate communication and information sharing Lack of collaboration between providers | Workforce shortages Insufficient education and training in MAT for OUD Need for high-quality clinical supervision Challenges with employee retention | Social stigma in the community Stigma from providers and staff Stigma against MAT within self-help groups | Patient barriers (e.g. transportation, childcare) Provider barriers (e.g. lack of time, regulatory burdens) | Limited resources and reimbursement Poorly aligned payment models and inadequate compensation Medicaid billing restrictions in some states/jurisdictions |
LESSONS LEARNED FROM CASE STUDIES
The five MAT programs visited were selected for their diversity and strong emphasis on psychosocial services. Several sites had created or re-designed their programs relatively recently and were still adjusting their service model. Most programs were taking measures to maximize efficiency and increase access to treatment through, for example, walk-in services, group medication management visits, or re-designing workflows. Several programs reported that a shortage of knowledgeable, trained behavioral health clinicians and limited space served as practical limitations on their ability to scale-up services. Success of the MAT program was often tied to the local context and whether the community has sufficient resources and supports for individuals with OUD.
In addition, some programs offered psychosocial supports that were very structured and standardized for all patients. Others were more patient-centered and tailored the treatment approach or allowed patients to choose their services and providers. Some programs incorporated "specialty tracks" for patient subgroups, such as pregnant and postpartum women, transition-aged youth, patients with PTSD, and patients with more complex psychiatric disorders. The lack of comparable outcomes data and small sample size prevents generalization of the findings from these case studies, yet they do illustrate a broad range of approaches to psychosocial supports in MAT.
Optimal Utilization of Psychosocial Support in Medication Assisted Treatment for Opioid Use Disorder
This brief was prepared under contract #HHSP233201600025I between HHS’s ASPE/DALTCP and Westat. For additional information about this subject, you can visit the DALTCP home page at http://aspe.hhs.gov/office-disability-aging-and-long-term-care-policy-daltcp or contact the ASPE Project Officer, Joel Dubenitz, at HHS/ASPE/DALTCP, Room 424E, H.H. Humphrey Building, 200 Independence Avenue, S.W., Washington, D.C. 20201. His e-mail address is: Joel.Dubenitz@hhs.gov
Reports Available
Optimal Utilization of Psychosocial Supports in Medication-Assisted Treatment for Opioid Use Disorder Issue Brief
- HTML https://aspe.hhs.gov/basic-report/optimal-utilization-psychosocial-supports-medication-assisted-treatment-opioid-use-disorder-issue-brief
- PDF https://aspe.hhs.gov/pdf-report/optimal-utilization-psychosocial-supports-medication-assisted-treatment-opioid-use-disorder-issue-brief
Psychosocial Supports in Medication-Assisted Treatment: Site Visit Findings and Conclusions
- HTML https://aspe.hhs.gov/basic-report/psychosocial-supports-medication-assisted-treatment-site-visit-findings-and-conclusions
- PDF https://aspe.hhs.gov/pdf-report/psychosocial-supports-medication-assisted-treatment-site-visit-findings-and-conclusions
Psychosocial Supports in Medication-Assisted Treatment: Recent Evidence and Current Practice (Appendix B)
