ASPE Report
Providing Medicaid to Youth Formerly in Foster Care under the Chafee Option: Informing Implementation of the Affordable Care Act
November 2012
By: Michael R. Pergamit, Marla McDaniel, Vicki Chen, Embry Howell, Amelia Hawkins
Abstract
This report draws lessons from 30 states’ implementation of existing optional Medicaid coverage for youth who age out of foster care and applies them to decisions and plans states will consider as they implement new ACA coverage that goes into effect in 2014. Wide variations in how states have implemented the so-called Chafee Option are focused on eligibility criteria, enrollment processes, and recertification processes. States’ implementation choices had implications for the frequency with which youth enroll in Medicaid coverage after foster care and in their continuity of coverage over time. The report also describes how states have approached and devised solutions to a series of implementation challenges such as coordinating data systems and forms, training staff about the new coverage, and helping youth maintain coverage.
Printer friendly version in PDF format (55 pages)
Acknowledgments
This report was prepared by the Urban Institute for the U.S. Department of Health and Human Services, Office of the Assistant Secretary for Planning and Evaluation (DHHS/ASPE) under Task Order No. HSP23337017T (UI Project 08350-017-00). Laura Radel was the task order officer and provided valuable guidance throughout the project and on the final report. We also thank the independent living coordinators and other child welfare staff for their time and input about providing Medicaid to youth aging out of foster care in their states. All errors are those of the authors.
Contents
- EXECUTIVE SUMMARY
- I. INTRODUCTION
- II. BACKGROUND
- III. HOW STATES HAVE IMPLEMENTED THE CHAFEE OPTION
- IV. THE EFFECT OF YOUTH PARTICIPATION IN ENROLLMENT ON THE LIKELIHOOD OF GETTING ENROLLED AND SEEING A PHYSICIAN
- V. LEARNING FROM THE CHAFEE OPTION: WHAT STATES MAY CONSIDER AS THEY IMPLEMENT THE AFFORDABLE CARE ACT
- VI. DISCUSSION
- REFERENCES
- APPENDIX A: Study Methodology
- APPENDIX B: Age-Out Policies by State
- APPENDIX C: Eligibility Criteria by State
- APPENDIX D: Enrollment Process by State
- APPENDIX E: Recertification Process by State
- APPENDIX F: State Summaries of Medicaid Processes under the Chafee Option
EXECUTIVE SUMMARY
Youth who age out of the child welfare system (i.e., reach majority age while in foster care) often face significant challenges as they transition to living on their own—especially with respect to health. Compared to their peers in the general population, they are more likely to have a health condition or disability that limits daily activity and to be in poorer overall health (Courtney et al. 2007; Courtney et al, 2011). They are also less likely to have health insurance (Courtney et al. 2011). This report details how 30 states have exercised a federal option through the Chafee Foster Care Independence Act of 1999 to expand Medicaid coverage to youth formerly in foster care until their 21st birthday (referred to as the Chafee Option).1 The report draws lessons from states’ implementation of the Chafee Option and applies them to decisions and plans states will consider as they implement the Patient Protection and Affordable Care Act (ACA) in 2014. Most relevant to child welfare agencies is the provision that, beginning in 2014, makes all youth who were in foster care on their 18th birthday eligible for Medicaid until age 26. We draw on published information supplemented by discussions with state administrators, staff, and informed advocates and find that states have designed and implemented the option in different ways that may potentially affect youth enrollment rates.
Eligibility, Enrollment, and Recertification Vary under the Chafee Option
Under the Chafee Option, states have some flexibility in determining eligibility. That includes deciding whether to require state residency rules or income and resource limits (that is, criteria for means testing), or whether to screen youth for alternative Medicaid coverage categories before considering them for Medicaid under the Chafee Option. Most of the 30 states that implemented the Chafee Option elected not to require income and resource limits. All states required that youth be state residents to qualify, and most would only cover youth who had been in foster care in their state.
States’ enrollment and recertification procedures under the Chafee Option can be categorized according to how much they required youth to be involved in the process. Half of the states (15) implemented procedures that did not necessitate youth involvement. States either developed an automated computer system that triggered an automatic enrollment, or they required child welfare caseworkers or a Medicaid specialist to enroll eligible youth. Twelve states required youth to work with their child welfare caseworkers to fill out and submit the application. Three states required youth to enroll on their own, as would any other individual applying for Medicaid.
Although under the Chafee Option youth are technically eligible for Medicaid until age 21, most states required some type of annual review, usually called “recertification,” to verify youths’ continued eligibility. In nine states, however, youth continued to be eligible without review until they turned 21. Among the states requiring annual review, 13 required direct youth action that ranged from providing address verification to turning in additional documentation (e.g., income verification). Eight states, on the other hand, required an annual review but with minimal or no youth involvement.
States’ Enrollment and Recertification Procedures May Affect Enrollment Rates
Using Medicaid enrollment and encounter data from FY2006–FY2008 from 10 states that had previously taken the Chafee Option, we found evidence that youth in states requiring more youth participation were less likely to enroll. The same was true with recertification. Although youth were more likely to be enrolled when they were required to do less, they were no more likely to have seen a doctor. Our findings suggest that as states implement the Affordable Care Act they may want to consider methods that reduce the burden on youth in order to maximize enrollment, but incorporate information about Medicaid benefits and the youths’ entitlement to Medicaid into their transitional services.
Important Considerations as States Implement the ACA
Based on what we have learned from the 30 states that took the Chafee Option, we highlight implementation lessons that may be relevant to states as they implement the Affordable Care Act. We do not advocate any specific direction; our goal is to present the issues that states should consider as they make their own decisions about implementation.
- Child Welfare and Medicaid Collaboration and Leadership. Implementing the Chafee Option was generally a joint effort by the child welfare and Medicaid agencies in each state. For the most part, states described the relationships as collaborative and emphasized the importance of both agencies communicating frequently—especially when setting up and designing their procedures.
- Coordinating Data Systems and Forms. Several administrators and staff advised that states should make their systems as automated as possible. Common recommendations included designing an interface between the Medicaid and child welfare data systems, so that Medicaid could identify when a youth had aged out of care or the child welfare agency would know when it was time to initiate the youth’s enrollment under the Chafee Option.
- Training Administrators and Front-Line Staff. Youth aging out of foster care represent a very small proportion of the Medicaid population. For Medicaid agencies this meant few staff members were knowledgeable about the Chafee Option. This also meant that child welfare staff had fewer people they could contact with questions. Providing ongoing training to Medicaid and child welfare administrators and staff was one solution proposed by states.
- Educating Youth. Regardless of how well the Medicaid and child welfare agencies collaborate or how seamless or automatic the enrollment process, providing coverage to youth formerly in foster care will have limited utility if youth do not see its importance or learn to access providers or seek care. Several administrators and staff discussed the importance of educating youth about maintaining health insurance coverage and keeping up with application forms and necessary documentation.
- Helping Youth Maintain Coverage. Helping youth formerly in foster care maintain coverage may present some challenges for states. One challenge has been determining how to assist youth once they are no longer involved with the child welfare agency (i.e., after they have turned 18, or up to 21 in some states); a second challenge has been finding ways to ensure youth know they are eligible as former foster youth, even if they are initially enrolled under a different coverage category (which is important if they lose coverage for any reason); and a third challenge has been devising procedures for maintaining coverage among a highly mobile population characterized by frequent moves and unstable living arrangements.
Discussion and Implications
The decisions made and lessons learned in implementing the Chafee Option have given states a good start in preparing to implement the Affordable Care Act provision to make youth who age out of foster care eligible for Medicaid until age 26. Certain holes exist, as not all eligible youth became enrolled under the Chafee Option and fewer remained enrolled over time. Furthermore, with the adoption of Affordable Care Act provisions, states will make several changes to their Medicaid systems. These provide new opportunities for meeting the needs of youth leaving foster care, but could also leave them at risk of falling through the cracks as states deal with the myriad complexities the law introduced.
One of the biggest challenges states will face in implementing the provision for youth formerly in foster care is keeping them aware of their categorical eligibility. That includes keeping youth aware, but also keeping service providers from other systems (e.g., mental health and substance abuse providers, TANF providers, criminal justice providers) aware of the provision.
Finally, the ACA provision represents a national requirement to provide Medicaid coverage to youth who age out of foster care. However, the child welfare system is managed within each state and no system exists for one state to know if a young person had been in foster care in another state. Whether states can coordinate in a way that prevents these youth from falling through the cracks is an open question.
I. INTRODUCTION
Youth who age out of the child welfare system (i.e., reach majority age while in foster care) often face significant challenges as they transition to living on their own—especially with respect to health. Compared to their peers in the general population, they are more likely to have a health condition or disability that limits daily activity and to be in poorer overall health (Courtney et al. 2007; Courtney et al. 2011). They are also less likely to have health insurance (Courtney et al. 2011). Our report details how 30 states have exercised a federal option through the Chafee Foster Care Independence Act of 1999 to expand Medicaid coverage to youth formerly in foster care until their 21st birthday (referred to as the Chafee Option). We draw on published information supplemented by discussions with state administrators and staff and informed advocates to examine how states have designed and implemented the Chafee Option. We describe and categorize implementation features and highlight aspects that could explain state differences in youth enrollment rates. We also report key findings from an analysis of Medicaid enrollment and encounter data in 10 states, which tested whether one implementation feature in particular—the extent that youth must participate in the enrollment process —explains state variation in enrollment at age 19 and at age 20, and the likelihood that youth see a physician between their 18th and 19th birthdays.
According to provisions established in the Patient Protection and Affordable Care Act (Affordable Care Act, or ACA), all youth who were in foster care on their 18th birthday will be eligible for Medicaid until age 26, starting in 2014.2 Significantly, the Affordable Care Act supersedes the Chafee Option, which covers youth until age 21. In conversations with states, administrators and staff described lessons they learned in implementing the Chafee Option. Based on the information gathered from published documents and conversations during the winter and spring of 2011, as well as analysis of Medicaid enrollment and encounter data, we discuss implications of states’ decisions and tradeoffs states may consider as they implement this provision of the Affordable Care Act. (See appendix A for detailed discussion of methods used in the study.)
II. BACKGROUND
Nearly 28,000 youth aged out of foster care in FY2010 (U.S. DHHS 2011). Many of the youth face significant challenges as they transition to living on their own—challenges exacerbated by limited education and employment experience, relatively poor mental and physical health, and a comparatively high likelihood of homelessness, incarceration, and teenage childbirth (Courtney et al. 2005; Goerge et al. 2002; Pecora et al. 2005).
Of particular concern are youth aging out of foster care who, lacking health insurance, may not seek or receive services for both acute and chronic conditions (English 2006). Under the Chafee Foster Care Independence Act of 1999 (FCIA), states have the option to provide expanded Medicaid coverage to youth who age out of foster care until they turn 21 (the Chafee Option). This option gives youth explicit eligibility for Medicaid based solely on their status as having been in foster care on their 18th birthday (see figure 1 for provisions). The program effectually makes health insurance an option for many youth formerly in foster care who would not have qualified otherwise. For example, prior to the expansion, low-income 19-year-olds in most states would not be eligible unless they were pregnant, had a dependent child (Schwartz and Glascock 2008), or met the conditions to stay in foster care past age 18 in states where that was an option. Prior to leaving care, youth in foster care are categorically eligible for Medicaid as foster youth, regardless of when they age out. Once they leave care they are eligible for the Chafee Option (until they turn 21).3
FIGURE 1. Chafee Option Provisions (42 U.S.C. 1396(a)(10)(A)(ii)(XVII))
Under the Chafee Foster Care Independence Act of 1999 (FCIA), states are given the option to provide extended Medicaid coverage to foster youth who age out of care or become “independent foster care adolescents” (i.e., The Chafee Option). By law states must define independent foster care adolescents as
- 21 years of age and
- foster care under the responsibility of a state on their 18th birthday.
Under the FCIA legislation states have the option to
- a limit on the assets, resources, and income the youth may have, as long as the levels do not exceed those established by a state for TANF on July 16, 1996;
- benefits only to those youth who had received Title IV-E foster care maintenance payments or independent-living services before their 18th birthday; and
- their definition of independent foster care adolescents to “reasonable categories” of youth.
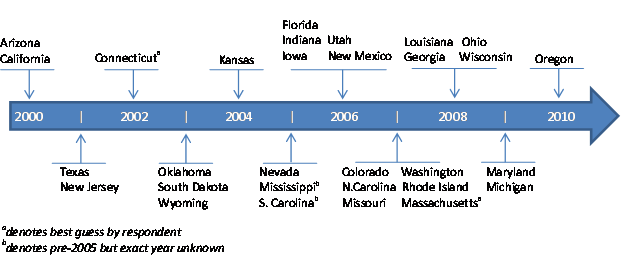
As of January 2011, 30 states had expanded Medicaid coverage to youth past age 18 through the Chafee Option (see figure 2). Over 70 percent of states that have taken the option took it around or after 2005.4 Although many states now have expanded coverage, very little is known about enrollment among youths formerly in foster care and how the provisions (including eligibility, enrollment, and recertification procedures) may affect who receives and retains health insurance.
Few empirical studies have examined procedural barriers to accessing and remaining enrolled in Medicaid specifically among youth formerly in foster care, although some critical reviews highlight the need for simple procedures to increase enrollment success (e.g., fewer requirements and seamless enrollment that prevents gaps in coverage as youth leave foster care) (English 2006). The focus on simplicity is frequently cited in research on access to health insurance by other low-income populations—particularly families with dependent children.
FIGURE 2. States That Took the Chafee Option by Year
Two common procedural barriers to enrollment in Medicaid and SCHIP among low-income families are difficulty navigating the enrollment and recertification process (Dorn 2007; Hanna, Radican-Wald, and Prater 2009; Kenney, Cook, and Dubay 2009) and unawareness about the program or eligibility requirements (Hanna, Radican-Wald, and Prater 2009; Kenney, Cook, and Dubay 2009; Perry and Betty 2010). Low-income parents of uninsured children report confusion about Medicaid and SCHIP eligibility requirements, which inhibits enrollment. They also describe “less urgency” to apply if they have older adolescent children (Perry and Betty 2010). Among a national sample of families, nearly 1 in 5 named administrative hassles (e.g., provision of documents, transportation) as a central reason why they did not apply (Kenney and Haley 2001).
Strategies associated with higher enrollment and successful applications include providing assistance from health care providers or community-based organizations (Dorn, Hill, and Hogan 2009), increasing outreach efforts (Dorn 2007), and simplifying the enrollment process —for example, forgoing face-to-face interviews and removing asset tests (Hanna, Radican-Wald, and Prater 2008). Some simplification procedures may not have the desired effect, however. Hill and Lutzsky (2003) note an increase in denied applications as a result of mistakes (i.e., incomplete or incorrect forms) with mailed-in applications. One lesson they draw is that easier is not always better.
Youth eligible for the Chafee Option may be affected by similar hurdles to enrollment as identified by families with dependent children. For example, like other potential enrollees, youth may be deterred if they find the eligibility rules confusing, are unaware of the option, experience administrative hassles, feel they do not need health insurance, or do not receive help with the application.
III. HOW STATES HAVE IMPLEMENTED THE CHAFEE OPTION
States have some flexibility in implementing the Chafee Option. They determine who is covered and how to define “reasonable categories” of youth formerly in foster care. Some states limit eligibility to citizens or state residents only, or choose to solely cover youth who were in foster care in their state. In some states, if youth are eligible for Medicaid for a reason in addition to having been in foster care (e.g., a pregnant youth exiting care), states may determine under which category the youth will qualify.
Enrollment procedures may vary as well. Youth may be required to enroll on their own at a Medicaid office or may fill out an application form at the child welfare office with help from their child welfare caseworker. In other states, enrollment is automatic. Youth are transferred from their prior Medicaid coverage to the Chafee Option coverage either on their 18th birthday or when they age out of care. The youth may not even know a change in coverage has occurred.
After initial enrollment the Medicaid agency periodically reviews all cases to make sure youth are still eligible. Some states require annual reviews or recertification. Other states forego annual reviews and permit youth to remain covered until their 21st birthdays —at which time they may reapply if they qualify under another coverage category. Below we describe in more detail these and other differences in eligibility and the enrollment and recertification processes.
ELIGIBILITY
As required by the FCIA legislation, every state that took the Chafee Option requires youth to have been in care on their 18th birthday.5 Some states allow youth to stay in care past the age of 18 (see appendix B for states’ age-out policies). In some of these states youth are transferred over to Medicaid under the Chafee Option on their 18th birthday, whether or not they leave care at that age. In other states youth are not transferred over to Medicaid under the Chafee Option until they leave care, which may occur after their 18th birthday (see appendix C for a description of eligibility criteria by state).
Several states discussed explicit definitions of “being in care [on the youth’s 18th birthday]” or the types of placements allowable for youth to be eligible for the program. In Colorado, youth need to have been in care on their 18th birthday in a “certified or licensed facility” and to have received maintenance or adoption assistance in the month of their 18th birthday. In Washington youth can be in licensed or unlicensed foster care, relative foster care, tribal foster care, Interstate Compact on the Placement of Children foster care (in Washington state), dependency guardianships established before 2010, or court-ordered placements. In Texas youth have to be in the state’s “Managing Conservatorship” at age 18. In Kansas youth in any of the following situations on their 18th birthday are eligible: foster home, relative or kin placement, group home, independent living, transitional living, secure care, a trial home visit, or AWOL or runaway status. Youth in Wisconsin must be in foster care (either foster care that is partially funded by the federal government under Title IV-E of the Social Security Act or non-IV-E foster care without federal participation), subsidized guardianship, or court-ordered kinship care under the care and supervision of the state, county, or tribe on the date that the youth turned 18. In Ohio the youth must have received independent-living services furnished by a program funded under Title IV-E.
Among states we spoke with, only Nevada explicitly reported to us that they require youth to be Title IV-E eligible to receive Medicaid under the Chafee Option. In Florida youth are categorically eligible for the Chafee Option if the child is eligible under Title IV-E of the Social Security Act for subsidized board payments, foster care, or adoption subsidies; however, Florida also extends eligibility to youth who are not IV-E eligible but are in foster care, shelter, emergency shelter care, or subsidized adoption. Washington and Wisconsin make explicit that youth in the adoption support program are ineligible.
States also vary as to when a youth’s coverage will switch eligibility categories from Medicaid as a ward of the state to coverage under the Chafee Option. Some states enroll youth in Chafee Option coverage when the youth turns 18 regardless of whether they continue in care or not; other states (for example Texas) offer Medicaid under the Chafee Option when foster youth leave care, which may occur after the individual’s 18th birthday. In Massachusetts youth must be in custody one day before their 18th birthday and in a placement for the six months prior to their birthday. This was the only state that described a minimum amount of time youth need to be in care.
Income and Resource Limits
Only a few states opted to include income and resource limits. In Maryland the income limit is 300 percent of the federal poverty level (FPL), in Indiana and Iowa 200 percent, and in Oklahoma 180 percent. Arizona had an income limit of 200 percent of the FPL, but eliminated it after 2000. In Texas, youth must be below 400 percent of the FPL and have less than $10,000 in resources. Independent-living coordinators and others we spoke with reported that the income and assets of former foster youth rarely exceed these limits. Their views are supported by data. For example, in Iowa, where youth cannot have incomes exceeding 200 percent of the federal poverty level, Courtney and Dworsky (2006b) find few 19-year-old youth who aged out of foster care in Iowa earn above that level (approximately 3–5 percent).
State Residency Rules
All states require youth to be a resident of the state while covered under the Chafee Option, and most states require youth to have been in care in the state on their 18th birthday to qualify for Medicaid under the Chafee Option. Consequently, most youth lose coverage if they move out of state, though they can regain coverage if they return. In Missouri, resident youth attending an out-of-state school or are temporarily outside of Missouri remain eligible; however, their out-of-state provider must be willing to accept MO HealthNet Medicaid. Unlike most states, Georgia, Texas, Louisiana, and Wisconsin will cover youth who were in a different state’s foster care system as long as they are current state residents.
SSI and Other Medicaid Coverage Categories
States generally have a hierarchy to determine how a youth qualifies for Medicaid. South Dakota, Massachusetts, and Oregon described enrolling youth in Medicaid under the Chafee Option without first determining their potential eligibility under other coverage categories.
The most common eligibility category to supersede the Chafee Option is Supplemental Security Income (SSI). In every state except South Dakota, Massachusetts, and Oregon, a disabled youth aging out of foster care who receives benefits through SSI generally receives Medicaid under SSI, not the Chafee Option. New Mexico, Arizona, and Mississippi all mentioned that youth exiting foster care might have been eligible for SSI Medicaid as a child but not under the stricter adult SSI eligibility rules. Several states, including Washington and the three states above, noted that should former foster youth be dropped from SSI Medicaid, they will be transferred to the Chafee Option with no break in coverage. In Arizona, child welfare staff will only submit the Chafee Option application if a youth is not first approved for adult SSI. Washington State described an automated process that flags all former foster youth who receive Medicaid through adult SSI. In the event the youth loses SSI coverage, a Medicaid worker would be alerted and after seeing the “former foster youth” tag, would know to transfer the youth’s eligibility category.
Several states described other potential Medicaid coverage categories under which former foster youth might also qualify. Utah, Arizona, New Mexico, and Texas indicated that a pregnant youth exiting foster care would receive Medicaid due to her pregnancy. Regarding parenting youth, Kansas, Arizona, and Texas reported that an eligibility worker would consider coverage under the Chafee Option or under a different Medicaid program for families. Similarly, youth in Oklahoma are screened for eligibility as low-income single individuals before getting enrolled as former foster youth.
In many states youth already covered by another Medicaid category will switch coverage to the Chafee Option. In Nevada, youth receiving Temporary Assistance for Needy Families (TANF) are ineligible for the Chafee Option. Similarly, in Washington, youth who apply for TANF can unwittingly undo their eligibility under the Chafee Option. To prevent this, an alert is sent if the youth’s record is touched. Texas and Missouri report that if youth have adequate coverage through a third-party resource (e.g., health insurance through an employer), they would not be eligible for the program. Missouri also reported that youth who choose to qualify under a different eligibility category will not also be considered for the Chafee Option. In Iowa, youth who are mandatory members of a covered household are ineligible; for example, if the youth has a child and applies for Medicaid for herself and her infant, the youth will not receive Medicaid under the Chafee Option but under the family Medicaid coverage group. These youth do maintain a flag in their record indicating that they would be eligible for Chafee if their family Medicaid is dropped. Similarly, in many states, including Arizona, Missouri, and Iowa, if the youth loses coverage under another category they are automatically reenrolled under the Chafee Option as former foster youth.
Other Requirements
States named a variety of other eligibility requirements to receive Medicaid under the Chafee Option. However, not every state highlighted the same criteria; so it is possible that other states, not mentioned below, have similar requirements.
States provide Medicaid to U.S. citizens or qualified aliens; however, California reported to us that Medicaid for undocumented youth aging out of foster care is covered by state funds.
Some states mentioned eligibility restrictions for their tribal populations. Tribal youth are ineligible in Arizona (though they are covered by a different category of state Medicaid) but are eligible in Washington and Wisconsin.
South Carolina reported they have no marital status restriction, meaning that eligibility for Medicaid under the Chafee Option may continue until age 21 without regard to the youth’s living arrangements.
ENROLLMENT
Below we discuss the ways states that took the Chafee Option enroll youth in Medicaid as they age out of foster care. We have organized the discussion to reflect the amount of participation and involvement required by the youth. States generally fall into three categories: those that do not involve the youth in the enrollment process, those that involve the youth with assistance from their child welfare caseworker, and those that require youth to enroll on their own. Other factors that distinguish states include whether Medicaid units are located within the child welfare agency and whether Medicaid enrollment forms are tailored specifically for foster youth. Some states also discussed the extent that they assist youth in locating providers. Table 1 shows how the states distribute across the three main categories of youth involvement in enrollment. See appendix D for a more detailed look at each state’s enrollment procedures.
TABLE 1: State Variation in Enrollment
| Youth is not involved | Caseworker assists youth | Youth enrolls on own |
|---|---|---|
| California | Arizona | Maryland |
| Colorado | Connecticut | North Carolina |
| Florida | Georgia | Wyoming |
| Indiana | Kansas |
|
| Iowa | Nevada |
|
| Louisiana | New Mexico |
|
| Massachusetts | New Jersey |
|
| Michigan | Ohio |
|
| Mississippi | Oklahoma |
|
| Missouri | Oregon |
|
| Rhode Island | Utah |
|
| South Carolina | Wisconsin |
|
| South Dakota |
|
|
| Texas |
|
|
| Washington |
|
|
Youth Is Not Involved in Enrollment
Several states have opted to design a process that places no enrollment requirements on youth. The youth becomes enrolled automatically and receives a Medicaid card (or retains the card he or she had as a foster youth). Among these states, there is some variation in how automatic enrollment occurs and whether the process relies on someone (other than the youth) to assist the enrollment. Nine states have automated the process by linking their Statewide Automated Child Welfare Information System (SACWIS)6 with their Medicaid data system; although even among those with linked systems there is variation in how the process works.
Automated system with no manual processes. Two states have an automated system that does not involve any manual processes. In Louisiana, if no communication occurs between the child welfare and Medicaid agencies, the Medicaid case remains open until age 21. In Missouri, when the case is closed, the system automatically moves the case into an electronically shared area, designed specifically for Medicaid under the Chafee Option, which will send the youth’s medical information to the state’s Medicaid system, MO HealthNet.
Automated system alerts case status changes. Some states have incorporated system alerts any time a case status is changed. When a case is closed (after the youth ages out), the Medicaid system receives an alert and puts the youth on Medicaid under the Chafee Option. In California,7 Texas, Florida, Michigan, and Washington, the Medicaid agency receives alerts directly from the child welfare information system or a similar administrative data system, prompting staff to check eligibility and enroll youth who have aged out.
Automated alerts and manual enrollment. In other cases, child welfare staff either receive the alerts and communicate with the Medicaid agency about the cases or enroll the youth themselves. Massachusetts’s child welfare IT department will send an electronic communication to the Medicaid office. South Carolina’s child welfare office will send a letter or e-mail to the Medicaid office. South Dakota, Rhode Island, and Colorado have linked their systems such that the child welfare staff are able to enroll the youth who age out of care into Medicaid under the Chafee Option themselves.
Manual enrollment but no youth involvement. Finally, there are states that have no automation at all but still do not involve the youth in the process. For example, in Indiana, the caseworker fills out an application that is sent to the Medicaid office. In Iowa, the caseworker will send the case information, which includes the most recent Medicaid application, other medical documents, and income and citizenship proof, to a single person in the Medicaid agency who works on all foster youth medical cases. All of these documents are already in the case file so the youth does not need to supply any information. In Mississippi, the caseworker will write to Medicaid that the case is closing and if the youth is over age 18, Medicaid will switch the youth onto Medicaid under the Chafee Option. These processes are all done without the youth needing to participate.
Youth Is Involved in Enrollment with Assistance from Caseworker
In many states, the caseworker and youth work together on the enrollment process. The degree of youth involvement varies by state; some states request the youth be present and aware of the enrollment process and forms, some require the youth to sign a form, and others ask the youth to provide documentation to show eligibility.
Caseworker and youth fill out forms together, but youth involvement is not required for processing. In the simplest cases, the caseworker or other child welfare staff and the youth fill out an application together, but the youth does not necessarily need to be present for the application to be completed. These states, New Mexico, Wisconsin, Oregon, New Jersey, and Connecticut, indicated that the youth should be present so they are aware of the form and medical coverage. Officials in these states felt that understanding how to fill out an application and maintaining medical coverage is a life skill and that youth should be present to learn about the process. In Oregon, Medicaid will send a packet to the youth’s specified mailing address; the packet must be deliverable but does not need to be returned.
In New Jersey, caseworkers will make a referral with youths or on behalf of youths. If they are not already enrolled upon exiting care, they can call a hotline number to enroll at any point before their 21st birthday. They do not need to provide any information beyond their name and basic identification information, nor do they fill out any paperwork. The Office of Adolescent Services will verify the youths’ eligibility internally by checking their Medicaid files from when they were in foster care.
Caseworker and youth fill out forms together, and youth signature is required. In other states youth are required to sign the application in their caseworkers’ presence. In Nevada, Arizona, Kansas, Ohio, and Oklahoma the youth and caseworker work together to fill out the application prior to youth exiting care, typically during their transitional planning period. The youth (and in some cases, the caseworker as well) signs the application, and the caseworker is charged with submitting the application to Medicaid. In Georgia, the caseworker notifies Medicaid informally which youth are aging out of care, but the youth are required to sign a third-party resource letter.
Caseworker assists youth in filling out the form and youth must provide or return additional documents. In Utah, the caseworker helps the youth fill out the enrollment form, which the youth must sign, and assists the youth in gathering the additional documents required. These documents include income, citizenship, identity, and social security number verification; evidence of citizenship and identity must be included with the enrollment form. Although there is no income limit for youth to enroll in Medicaid under the Chafee Option, Utah policy restricts coverage only to those not eligible for Medicaid under all other eligible groups. Once completed, the caseworker will send the application to Medicaid Eligibility with all additional documentation.
In Wisconsin, a caseworker will assist the youth in filling out the standard Medicaid application prior to exiting care. Once the Medicaid agency receives the information, the Medicaid agency mails a Medicaid HMO packet to the youth; the youth is not enrolled until he or she has returned the Medicaid HMO packet and selected a health plan.
Youth Enrolls on His or Her Own
Three states require the youth to bear the full responsibility for enrolling in Medicaid.
Youth goes to the local Medicaid office to enroll. In three states, the youth must go to the local Medicaid office and enroll using the standard Medicaid application process. In Wyoming, the independent-living coordinators can encourage and remind the youth to enroll, but it is still up to the youth to fill out the application and take it to the Medicaid office, which is housed in the same building as the child welfare office. Similarly, in Maryland and North Carolina, youth are expected to go to the county Medicaid office and enroll. North Carolina is trying to incorporate more information about Medicaid enrollment into the exit meetings caseworkers hold with youth in the weeks before they exit foster care.
Other Factors Related to Enrollment
Medicaid units located within child welfare. Some states have a special Medicaid unit located within the child welfare agency that handles enrollment and is also a resource for youth when they have questions. These states include Connecticut, Missouri, Rhode Island, and South Dakota. Other states, including Connecticut, Iowa, and Washington, have staff located within Medicaid that focus on foster children or have someone who is a point person for Medicaid for foster children. In addition, Iowa has one worker dedicated to processing all cases in their Medicaid for Independent Young Adults program.
Tailored enrollment application forms. Some states use regular Medicaid application forms for enrollment under the Chafee Option. Other states, particularly those where youth and caseworkers collaborate on the enrollment process, have tailored applications that have been shortened and simplified specifically for Medicaid under the Chafee Option. These states include Connecticut, New Mexico, Nevada, Arizona, and Kansas. Often these tailored forms are only one page and typically ask no income or household questions since those are irrelevant to these youths’ eligibility. Ohio has a simplified form but also requires two additional forms to be filled out (to determine eligibility for the Supplemental Nutrition Assistance Program (SNAP) and other welfare benefits). Wisconsin requires a full Medicaid application, though the form asks whether anyone in the household was in foster care on his or her 18th birthday.
Assistance and Other Supports Finding a Provider
States provide different levels of support and assistance to youth who have questions or need help finding a provider that will accept Medicaid. In some states, youth are encouraged to call their caseworker or another person in the child welfare agency with whom they feel connected. For example, Louisiana contracts with independent-living services providers and hope that the youth feel comfortable asking them their medical questions. Oklahoma has the Yes-I-Can hotline, available for youth aging out to ask any questions relating to independent living. In other states, the youth must call the Medicaid office to ask questions or to get help finding a provider. Typically, these states have a Medicaid support hotline already in place for all of their Medicaid enrollees and therefore are already equipped and ready to answer any enrollee’s questions. These states include California, Florida, Indiana, Iowa, Massachusetts, and Mississippi.
A few states, including Connecticut and Texas, have a single point person for former foster youth to call for any questions relating to Medicaid. Utah assigns each youth a nurse. Some states, such as Washington, Colorado, and Missouri, note that providers could look up youth in the Medicaid computer system if youth forget or lose their card. However, it was sometimes unclear how willing and able providers were to do so and whether this was common knowledge for youth aging out of care.
RECERTIFICATION
Although most states require an annual recertification to maintain Medicaid enrollment, nine states that have implemented the Chafee Option do not. In those states, youth have Medicaid coverage from their enrollment at their 18th birthday until their 21st birthday and are able to maintain the same card. At any time, youth may contact the Medicaid office to notify them of a change in address or to ask for a replacement card; however, they are never required to contact the Medicaid office. The state’s Medicaid system will indicate that the youth are eligible until their 21st birthday.
The remaining 21 states that took the Chafee Option require an annual review to verify youths’ eligibility. In 8 of the 21 states, however, recertification is “passive,” that is, the state sends out notifications or letters to check for any changes but the youth are not required to return them. If the notice is not returned, it is assumed that no changes have occurred. In contrast, the other 13 states require a more “active” recertification. Table 2 shows which states have a regular annual recertification (including “active” and “passive”), and which do not require recertification.
TABLE 2: State Variation in Recertification
| States That Require Annual Recertification | States That Do Not Require Annual Recertification | |
|---|---|---|
| Active Recertification | Passive Recertification | |
| Arizona | Florida | Colorado |
| California | Kansas | Louisiana |
| Connecticut | North Carolina | Massachusetts |
| Georgia | Oregon | Michigan |
| Indiana | Rhode Island | Mississippi |
| Iowa | South Dakota | Missouri |
| Nevada | Texas | New Jersey |
| Maryland | Ohio | South Carolina |
| New Mexico |
| Washington |
| Oklahoma |
|
|
| Utah |
|
|
| Wisconsin |
|
|
| Wyoming |
|
|
See appendix E for a more detailed description of each state’s recertification process. Below we describe the recertification procedures among the 21 states that require annual recertification grouped according to what is required of the youth.
Annual Review with Minimal or No Youth Involvement
Eight states require an annual review but require minimal or no participation from youth.
Internal recertification process. In four of the eight states, the renewal process is automatic from the youth’s perspective. In these states, the recertification is performed by someone other than the youth. In Florida, the Medicaid agency will check the child welfare agency’s information system annually to see if the youth has moved or passed away. In Kansas, the Medicaid agency will contact the caseworker with the assumption that the youth continues to keep in touch with the caseworker. In the case of no contact between youth and caseworker, Medicaid will keep the case open. In North Carolina, the Medicaid caseworker is responsible for the annual recertification, and in Rhode Island, it is assumed that the youth will update his or her address whenever necessary.
Passive recertification process. In the other four states, Oregon, South Dakota, Texas, and Ohio, the Medicaid agency sends the renewal to the youth’s address on file requesting address verification. If no response is received, the Medicaid agency will assume there has been no change and Medicaid coverage continues. Ohio sets up a telephone interview with the youth to check that the youth’s address has not changed and the youth is not incarcerated. The state only terminates Medicaid coverage if it is known that the youth is ineligible; otherwise, the case will remain open.
Annual Review with Youth Involvement but No Required Documentation
Some states involve the youth more directly but do not require them to provide additional documentation for recertification.
Youth must respond to notification form to remain enrolled. In six states (Arizona, California, Connecticut, Georgia, Wisconsin, and Wyoming), the youth is sent a form by the state Medicaid office and is required to respond. These states check for any address changes or youth who have moved out of the state and are no longer eligible. In these cases, income is not a factor to youth continuing to receive Medicaid benefits.
Recertification forms. Of these six states, only California has a tailored recertification form that is sent specifically to youth eligible for Medicaid through the Chafee Option. This form is a simple one-pager asking for identification information such as name, address, date of birth, social security number, and a signature verifying the youth’s acknowledgement of desiring to continue coverage. The other five states send their standard benefits recertification form, which allows the recipient to reenroll in Medicaid, food stamps, and other welfare benefits. These forms have sections on income, assets, household composition, and so on. The forms for Connecticut and Georgia ask for proof of income, such as a paystub, to be sent with the recertification form, while the other three states’ forms ask the recipient to report income to the best of their knowledge and sign a statement of truth. None of these states has an income requirement for their Medicaid under the Chafee Option. Some states reported that the youth did not need to fill out the income section to continue their Medicaid coverage but may need to if they are receiving other benefits with an income requirement.
Modes of response. States allow youth to recertify in several different ways. For example, Arizona allows youth to respond via mail, phone, online, or in person; in Georgia, youth can also fax the form. Most states, however, expect the forms to be mailed back.
Timeframe for returning form. Youth are required to return the form within a certain time period; otherwise their coverage is terminated. Typically, the form is sent out approximately 45 days prior to closure of coverage. Some states, such as California, will attempt to locate the youth through phone calls and other letters; other states including Georgia and Wisconsin will send a second reminder notice. If youth lose coverage, they must reapply—this process might involve simply calling the Medicaid office for reinstatement of coverage or it might require going to the Medicaid office and reapplying through a standard application.
Annual Review with Youth Involvement, Including Required Documentation
Seven states require a recertification form and additional documentation. Five of these, Indiana, Iowa, Nevada, Oklahoma, and Maryland, have income requirements for youth qualifying through the Chafee Option; the states therefore must verify that a youth is still eligible according to the income ceiling. The states send the youth a standard Medicaid application (Utah, Oklahoma), a standard welfare benefits application including Medicaid and food stamps (Iowa, Nevada), or an application tailored for former foster youth on Medicaid under the Chafee Option (New Mexico).8
New Mexico’s form is sent by the child welfare agency (Division of Youth, Children, and Families); youth will typically work with their transition specialists to fill out the form—they are asked to provide documentation for identification, citizenship, and any other health insurance coverage they may have. In Indiana, youth can seek help from their independent-living coordinators or caseworkers. Some of these states will send second reminder notifications, but other states (for example, Iowa) do not provide any follow-up calls or letters. All of these states except New Mexico check for address changes and income for continued eligibility.
Of these states, Iowa and Utah ask for proof of income to be attached to the recertification forms. The others ask the youth to sign a statement of truth.
IV. THE EFFECT OF YOUTH PARTICIPATION IN ENROLLMENT ON THE LIKELIHOOD OF GETTING ENROLLED AND SEEING A PHYSICIAN
A key feature of states’ implementation of the Chafee Option was the extent they involved youth in the enrollment process. Half of the states that took the option had designed procedures that did not require youth to be involved in initial enrollment. Most of the remaining states involved youth to varying degrees with assistance from a caseworker. Only three states reported that youth must apply for Medicaid under the Chafee Option on their own (table 1). Similarly, we saw three different recertification models that differed according to the level of youth involvement. One set of states required no recertification before age 21 (and therefore no youth involvement). Another set required an annual recertification but did not involve the youth (see “passive” recertification above); and a third group required youth to handle recertification on their own (table 2).
Using Medicaid enrollment and encounter data from FY2006–FY2008, we examined whether youth residing in states that required more effort to enroll were less likely to be enrolled. To test whether involving youth in the enrollment process led to youth being better informed about their Medicaid enrollment and benefits, we also examined whether increased youth involvement led to greater likelihood of using health care services, specifically seeing a physician.
Among the 30 states that took the Chafee Option as of January 2011, 10 met three criteria we imposed for inclusion in the analysis. First, to observe youth while in foster care and after at least one recertification point, states needed to have implemented the Chafee Option by FY2006 (data were available through FY2008). Second, states needed sufficient numbers of youth in foster care turning 18 in FY2006. And third, we needed states that could distinguish in their administrative data between youth who had been in foster care and youth who had been adopted. To be appropriate for the analysis, youth needed to have been eligible for Medicaid under the Chafee Option, which meant they needed to be in foster care on their 18th birthday. The 10 states included in the analysis were Arizona, California, Florida, Indiana, Iowa, Kansas, Nevada, South Carolina, Texas, and Utah. Although not necessarily nationally representative, the group includes states of various sizes. More detail on the sample can be found in appendix A.
Table 3 shows the enrollment and recertification processes for these 10 states. None required youth to enroll entirely on their own at initial enrollment. The states either did not require youth involvement or required some involvement with assistance from caseworkers. For recertification, states fell into four categories: (1) no recertification, (2) no youth involvement in recertification (or passive recertification when lack of an address update did not disqualify youth), (3) youth required to update address information, and (4) youth involvement in recertification, including a requirement to provide additional documentation such as income verification.
TABLE 3: States’ Enrollment and Recertification Processes
| Enrollment Process | Recertification Process | ||||
|---|---|---|---|---|---|
| No youth involvement | Youth involvement | No recertification | None required or passive | Annual address update | Annual income documentation |
| California Florida Indiana Iowa South Carolina Texas | Arizona Kansas Nevada Utah | South Carolina | Florida Kansas Texas | Arizona California | Indiana Iowa Nevada Utah |
Key Findings
We examined whether states requiring more youth participation in enrollment and recertification had lower rates of Medicaid enrollment one and two years later.9 We also examined whether more youth in those states visited a physician within one year. Each of the models controlled for demographic factors, diagnoses, and the percentage of youth in foster care at age 18.10 More detail about the methods, descriptive statistics, and findings can be found in Pergamit et al. (2012). Key findings include:
- Youth in states that required more participation in enrollment were 13.5 percentage points less likely to be enrolled in the month before their 19th birthday than youth in states that did not require their involvement.
- Youth in states that required participation in recertification were at least 5 percentage points less likely to be enrolled in the month before their 20th birthday than youth in South Carolina, which does not require recertification. Youth in states that required income documentation had the lowest recertification rates, 11 percentage points lower than in South Carolina. Although these findings held for most of the states for which data were analyzed, results for two states, Arizona and California, did not conform to the expected order. Despite requiring address updates, without which the youth would lose eligibility, these states showed recertification rates similar to South Carolina, which did not require any action by youth to maintain enrollment until their 21st birthday. It is unclear why these two states appear to recertify youth at higher rates than would be expected. Arizona provides multiple means for recertification (mail, online, in-person, phone) which may make recertifying relatively easy, however other states offer multiple methods, too. California uses a simplified form. In addition, counties in California are required to conduct due diligence in locating youth who do not respond to the recertification notice, including phone calls and additional letters. They also allow youth to be reinstated through an “easy” phone call if they fall off the rolls due to nonresponse. Interestingly, as seen in figure 2, Arizona and California were the first two states to implement the Chafee Option.
- Youth in states that required more participation in enrollment were no more likely to have seen a physician during the year after their 18th birthday. We tested whether youth in states that required youth participation in the enrollment process were more likely to visit a physician in the year after their 18th birthday than youth who were automatically enrolled. We did not find evidence of more physician visits among these youth. However, one should be cautious in interpreting this finding. States that automatically enroll youth may make youth aware of their benefits through other means. Alternatively, states that involve youth in the enrollment process may not adequately explain Medicaid benefits.
Our findings suggest that as states implement the Affordable Care Act, to maximize enrollment, they may want to consider methods that reduce the burden on youth but incorporate information about Medicaid benefits and the youth’s entitlement to Medicaid into their transitional services. Transitional services, generally available to youth formerly in foster care until age 21, may be important for helping youth maintain their Medicaid coverage (e.g., assisting with recertification, helping resolve enrollment problems). Given that under the Affordable Care Act youth will be eligible for Medicaid until their 26th birthday, however, we do not know if the enrollment patterns observed between ages 18 and 20 will apply after the youth are no longer eligible for transitional services.
V. LEARNING FROM THE CHAFEE OPTION: WHAT STATES MAY CONSIDER AS THEY IMPLEMENT THE AFFORDABLE CARE ACT
Based on what we have learned from the 30 states that took the Chafee Option, we highlight lessons that may be relevant to states implementing the Affordable Care Act provision on coverage for youth who age out of foster care. We do not advocate any specific direction; our goal is to present the issues that states should consider as they make their decisions about implementation.
The Patient Protection and Affordable Care Act, (P.L. 111-148) (Affordable Care Act, or ACA) is expected to substantially increase health insurance coverage among young adults in the general population, as well as young adults formerly in foster care. Currently, individuals ages 19–29 have the highest rates of uninsurance among adults under age 65 (Collins and Nicholson 2010), but several provisions in the Affordable Care Act are anticipated to address the disparities. Beginning in 2010 but required by 2014, many larger employers began offering health insurance for dependent children until age 26. By 2014 all adults with incomes less than 138 percent of the federal poverty level (the low-income group) will qualify for Medicaid in states that choose to implement this expansion.11 Unlike other coverage groups, youth formerly in foster care will be eligible until age 26, regardless of income. Youth formerly in foster care will receive a comprehensive benefits package that includes early and periodic screening and diagnostic and treatment services, compared to the “essential health benefits” offered to other young adults (Kenney, Pelletier, and Blumberg 2010). The federal government will pay the total costs for all newly covered individuals in the low-income group from 2014-2016—gradually reducing to 90 percent of costs in 2020 and thereafter (Kaiser Family Foundation 2012). However, the federal government will only reimburse coverage of youth formerly in foster care at the state’s regular, much lower, Federal Medical Assistance Percentage rate (Baumrucker et al. 2012).
Beyond plans and costs associated with expanding Medicaid coverage to young adults generally, states may require additional coordination and consideration as they prepare to cover youth formerly in foster care. In particular, expansion will entail collaboration between Medicaid and child welfare agencies to identify, enroll, and support youths’ coverage and their knowledge about eligibility and benefits. Below we discuss lessons shared by states that implemented the Chafee Option. Lessons that may be useful as states prepare to extend coverage to age 26 include those about agency collaboration and leadership, coordinating data systems and forms, training administrators and staff, educating youth, and helping youth maintain coverage over time. We also summarize a menu of potential enrollment and recertification procedures states described in implementing the Chafee Option.
Child Welfare and Medicaid Collaboration and Leadership
Implementing the Chafee Option was generally a joint effort by the child welfare and Medicaid agencies in each state. For the most part, states described the relationships as collaborative and emphasized the importance of both agencies communicating frequently—especially when setting up and designing their procedures. States with county-run child welfare agencies described additional challenges with standardizing and managing procedures across jurisdictions. Some recommendations for educating counties and county agencies included doing so through letters, standard guidelines and rules, and quarterly trainings.
A few people advised that getting buy-in from high-level leadership was important to ensure implementation was a priority. In some cases it meant educating policymakers and Medicaid officials about youth in foster care—for example, that “they [youth] didn’t do anything wrong” and that expanded coverage could potentially reduce health care costs, as youth without coverage would alternatively use hospital emergency rooms, which are generally more costly.
Several respondents mentioned that their states got started by assembling work groups with representatives from Medicaid, child welfare, health care providers, and other advocates or third parties such as state youth advisory councils, foster youth alumni, community advocates, and other health officials. Information technology and other systems professionals were often included in the design and planning.
Regarding ongoing collaboration, states varied in the extent the child welfare and Medicaid agencies interacted once the Chafee Option was in place. This may have implications for how effectively states communicate eligibility and enrollment information to youth and staff. At one end of the spectrum, child welfare staff had little or no contact with the Medicaid agencies. When asked who they would contact with a question about eligibility or enrollment, child welfare staff would consult the Medicaid agency’s web site —as any other recipient might. In other states, child welfare staff had a Medicaid liaison or even an office within the child welfare agency that could address health insurance questions. In all states, youth formerly in foster care were a small coverage group compared to the general Medicaid population; child welfare officials suspected that few Medicaid staff, particularly in local offices, would know about the Chafee Option. As a consequence, child welfare officials expressed some concern that unless child welfare and Medicaid staff knew who to contact with questions, youths’ needs may go unmet—or the lack of knowledge would present additional obstacles to enrollment.
Coordinating Data Systems and Forms
Several administrators and staff advised that states make their systems as automated as possible. Common recommendations included designing an interface between the Medicaid and child welfare data systems (see the Enrollment and Recertification sections above for examples) so Medicaid could identify when a youth had aged out of care or the child welfare agency would know when it was time to initiate the youth’s enrollment under the Chafee Option. Not every state linked their data systems, although many wished they could. Another recommendation was to develop procedures and systems that utilized structures already in place so states were not building the infrastructure from scratch. Some states created tailored application forms or added questions to existing forms to distinguish youth formerly in foster care. Another recommendation was to have the application forms available at the child welfare agency, since it eases access by youth and their caseworkers.
Training Administrators and Front-Line Staff
As mentioned earlier, youth aging out of foster care represent a small proportion of the Medicaid population. For Medicaid agencies this meant few staff were knowledgeable about the Chafee Option. For child welfare offices, this also meant staff had fewer people they could contact with questions. Ongoing training for Medicaid and child welfare administrators and staff was one solution proposed by states. To educate child welfare staff, administrators would hold internal trainings, make regular announcements about the provision at staff meetings, and use video conferencing to alert offices to policy changes. Staff turnover at both the child welfare agency and Medicaid offices was a challenge to keeping local offices informed. One consequence of staff not knowing about the Chafee Option is that when enrollment is not automatic, eligible youth may be turned away by Medicaid or not informed by their child welfare caseworker that they can and should apply. States stressed the need to make sure information and procedures get disseminated and the process is as seamless as possible.
Educating Youth
Regardless of how well the Medicaid and child welfare agencies collaborate or how seamless or automatic enrollment is, coverage for youth formerly in foster care will have limited utility if youth do not see its importance, learn to access providers, or seek care. Several administrators and staff discussed the importance of educating youth about maintaining health insurance coverage and keeping up with application forms and necessary documentation. They advised states to discuss health insurance early in the transition planning process. One official said the state did not wait until a youth was about to turn 18 to begin the conversation, but encouraged workers to talk about coverage as early as age 14. Some considered enrollment as a vital life skill and would teach youth how to talk to receptionists at the Medicaid office (if that is where they apply). States also described teaching youth how to select a provider and set up an appointment. Others suggested that information about eligibility and application should be posted in places youth will see it. These might include foster youth alumni club web sites, child welfare department web sites, transitional living programs, youth shelters, public health clinics, and youth conferences. Education was especially important in states that did not have automatic enrollment, although youth in states with automatic enrollment arguably should know about the coverage as well, in order to get the care they need.
Helping Youth Maintain Coverage
Helping youth formerly in foster care maintain coverage may present some challenges for states. Administrators and staff gave three examples from their experiences implementing the Chafee Option. One challenge has been determining how to assist youth once they are no longer involved with the child welfare agency (e.g., after they have turned 18, or up to 21 in some states). A second challenge has been finding ways to ensure youth know they are eligible as former foster youth, even if they are initially enrolled under a different coverage category (which is important if they lose coverage for any reason). A third challenge has been devising procedures for maintaining coverage among a highly mobile population characterized by frequent moves and unstable living arrangements.
After Contact with Child Welfare Ends
Child welfare agencies may lose contact with youth at age 18, or by 21 for youth who stay in care or continue to receive transitional services. Therefore, administrators and staff from the child welfare and Medicaid agencies need to consider what steps they will take to ensure youth are aware of their eligibility and how to apply or recertify once they are no longer connected to the child welfare system. In implementing the Chafee Option, states were aware of the challenge and emphasized the importance of making sure youth are fully informed before they have left care. Solutions other states devised included keeping youth enrolled until age 21 without requiring an annual recertification. This solution may be somewhat effective for states implementing the Affordable Care Act, although they will need to consider what happens after youth turn 21 and whether keeping youth continuously enrolled until age 26 is an option.
If Youths’ Medicaid Coverage Category Changes
Although youth may have been eligible for the Chafee Option when they turned 18, some may have been enrolled under other coverage categories if those categories took precedence (see the SSI and Other Medicaid Coverage Categories section above). In most cases, if youth lost coverage under their initial coverage category (e.g., pregnant youth), they would still qualify as former foster youth. Under the Affordable Care Act youth will be eligible regardless of income. If they qualify initially under another coverage category, for instance a category based on income, then lose their eligibility under that category, they should still qualify as former foster youth until they reach age 26.
States may need to consider procedures for preventing youth from inadvertently losing coverage when they continue to be eligible. With the Chafee Option, some states described default settings in their Medicaid systems that flagged youth who were formerly in foster care. If youth lost their initial coverage, it was possible for the Medicaid office to see that they had formerly been in foster care and would still qualify.12
If Youth Move or Have Unstable Housing
Youth aging out of foster care are a highly mobile population. Often their housing and living arrangements are precarious and unstable (Courtney et al. 2010). Maintaining health insurance coverage may be challenging whether the youth is moving to a nearby community, across counties, or across states. States may consider how to address unstable housing and the increased risk that youth in foster care may experience homelessness after leaving care.
Local moves. States described examples of youth moving to a new address and losing coverage because they did not keep their address information up to date with the Medicaid agency. In some states, the Medicaid office contacted the child welfare agency to follow up with the youth, under the assumption that youth stay in contact with the child welfare agency. Other procedures included maintaining the youths’ coverage even if they did not respond with updated address information (see the Passive Recertification Process section above). Other states elected not to require annual recertification to minimize dropped coverage due to frequent moves.
County moves. Sometimes a move will mean the youth’s health care provider changes. This was particularly relevant in states with county-based managed care systems or states with both fee-for-service and managed care systems.13 Youth would need to identify a new managed care provider and know enough about the county to understand which health insurance system was in place. Some states encouraged youth to stay in touch with their transitional living services coordinators and caseworkers so they could help answer questions such as these. Others provide contact information for the Medicaid agency and encourage youth to follow up with questions. States may need to ensure youth can access Medicaid staff familiar with their special eligibility as youth formerly in foster care (which means they do not have income limits and they qualify for the comprehensive benefits package).
Interstate moves. Youth may move to another state. Under the Chafee Option states could determine whether they would cover youth in foster care in a different state (see the State Residency Rules section above). This becomes a different issue under the Affordable Care Act when provisions are not voluntary. States must consider how they will coordinate to ensure youth are covered, even if they were not in foster care in the state where they currently live. Some states did not have systems in place to verify whether a youth was in foster care in another state. Youth will also need to be educated about their eligibility even if they move to another state.
Designing Enrollment and Recertification Procedures
As states plan to implement Medicaid expansion in 2014, they will make procedural decisions about day-to-day operations. Below we list enrollment and recertification features states described in implementing the Chafee Option. Although presented in tables 4 and 5 as a menu of possible options, the choices and procedures states design face various constraints. Factors such as the capacity of their administrative data systems, the size of their child welfare and Medicaid populations, organizational structure of their state and county governments, workforce capacity and staffing, financing and budgetary considerations, and political will play important roles. Still, the menu below demonstrates the wide spectrum that currently exists and the flexibility states have to customize procedures. Additional options are possible, but key features states will likely consider as they design their enrollment guidelines include the extent of youth involvement, the application form, the mode of applying, and the level and mode of communication across agencies (table 4). The range in youth involvement could vary from no direct involvement at all to complete responsibility for enrolling. The application form could be customized especially for the youth or be identical to the forms other Medicaid applicants use. States described several ways youth could apply: some used multiple methods (e.g., online, by phone, in person) while others found efficiency through limiting the ways youth could apply (e.g., applications are collected and submitted by the child welfare agency). Lastly, states communicated across agencies in different ways including shared access to data systems and other electronic communication, physically placing staff within the other agency, or having little cross-agency communication at all.
Recertification involves additional variables, including how to inform the young adults about procedures and how to continue making health care accessible once they are no longer involved with the child welfare system. Based on features states implemented through the Chafee Option, we anticipate similar considerations will be necessary for the Affordable Care Act, including the extent of youth involvement and consequences if youth fail to return applications, mode of applying, how the Medicaid agency contacts and communicates with the youth, and what role the child welfare agency plays. As with enrollment, states may design procedures that minimize or maximize the youth’s involvement or retain or drop a youth from Medicaid who fails to return his or her application.
TABLE 4: Examples of Enrollment Process Options
| ENROLLMENT FEATURE | PROCESS OPTION |
|---|---|
| Youth involvement
|
|
| Application form
|
|
| Mode of applying
|
|
| Interagency communication |
|
TABLE 5: Examples of Recertification Process Options
| RECERTIFICATION FEATURE | PROCESS OPTION |
|---|---|
| Youth involvement
|
|
| Consequences for youth who fail to return application:
|
|
| Mode of applying
|
|
| Contact/ communication |
|
| Child welfare agency role:
|
|
VI. DISCUSSION
Thirty states have implemented the Chafee Option. These states have designed and implemented Medicaid under the Chafee Option in a variety of ways. Although states stayed within the policy provisions established under the Chafee legislation, they exercised considerable discretion with respect to eligibility, enrollment, and recertification. Regarding eligibility, states set their own residency requirements and income and asset limits, and also determined whether they would screen former foster youth for alternative Medicaid coverage categories before considering them for Medicaid under the Chafee Option. Enrollment procedures varied considerably by state as well—ranging from states that required youth to enroll on their own to states that enrolled youth automatically with no youth involvement. Other features include the type of application form used (if any), whether there is a Medicaid assistance office within the child welfare agency, and how much help youth could receive in locating providers. States designed varying recertification policies that include whether or not an annual recertification is required and how much effort is required of the youth. A summary of the eligibility, enrollment, and recertification processes for each state that has implemented the Chafee Option can be found in appendix F.
The decisions made and lessons learned in implementing the Chafee Option have helped states start preparing to implement the Affordable Care Act provision to make youth who age out of foster care eligible for Medicaid until age 26. Certain holes exist, as not all eligible youth became enrolled under the Chafee Option and many of those did not remain enrolled over time. Furthermore, when adopting provisions of the Affordable Care Act, states will make many changes to their Medicaid systems. These changes provide new opportunities for meeting the needs of youth leaving foster care, but also could leave them at risk of falling through the cracks as states deal with the myriad complexities the law introduced.
One of the goals of this report is to help states choose how to implement the provision regarding coverage for youth who age out of foster care. It is not intended to propose a particular solution but to help each state identify the solution that best fits its situation. Input from the child welfare agency in determining the process as it is developed is critical for supporting the needs of this vulnerable population. In states that implemented the Chafee Option, a small number placed the entire responsibility and authority for developing procedures with the Medicaid agency with little or no involvement from the child welfare agency. In these states, the Medicaid agency typically tried to make the enrollment and recertification process for these youth fit into the existing Medicaid framework, disregarding these youths’ particular situation. As states tackle the many issues required to operationalize the Affordable Care Act, there is even more possibility that a group as small as former foster youth may be incorporated in a way that minimizes the burden to the Medicaid agency at the group’s expense. Good communication and ongoing collaboration between the Medicaid agency and the child welfare agency will be required to devise the appropriate procedures for these youth.
As states design procedures for implementing the Medicaid expansion, they may consider potential tradeoffs of different approaches. What’s better, the “simple” approach to enrollment (with no youth involvement) or the “life skills” approach? The evidence demonstrates that automatic enrollment is more likely to ensure initial high enrollment. However, in using this approach, youth may not be aware of benefits or seek care when needed. The “life skills” approach offers the child welfare agency an opportunity to inform youth about their benefits, how to find a provider, issues in maintaining good health and accessing health care when needed, and the decision to access a physician or clinic instead of using a hospital emergency room. However our analysis found that youth in states without automatic enrollment were less likely to be enrolled and were no more likely to visit a physician. To help inform youth of their benefits, states using automatic enrollment can build elements into their transition planning.
With respect to recertification, states can choose between having no recertification or having an annual review. A potential advantage of no recertification is that it is likely to help maintain enrollment over time. As with the “simple” enrollment approach, a potential disadvantage is that youth may not be aware of benefits. Over time, youth may lose sight of their Medicaid enrollment if they haven’t had to face recertification and if they have not accessed health care, leading them to access emergency rooms instead of practitioners or forgo care when they need it. Unlike the enrollment period, agencies may no longer have any direct contact with youth to reminders them about Medicaid coverage. On the other hand, recertification requirements may reduce take-up. The extent of youth involvement may affect awareness; the more youth must do, presumably the more they’re aware of their enrollment. Having dealt with recertification may help them maintain their enrollment after they are no longer connected with the child welfare agency. However, youth leaving foster care are a mobile population. Youth who move frequently may be more likely to lose coverage to the extent that recertification requires regular contact and update of address information.
These decisions may have become even more complicated as many states have begun to integrate applications for multiple benefit programs; particularly TANF, SNAP, and Medicaid. On the one hand, a single application (and recertification) may provide an opportunity for youth to access public benefits after leaving foster care. On the other hand, the application requirements for accessing these other benefits, including providing income documentation, may discourage youth from completing a process that is not necessary to enroll only in Medicaid.
One of the biggest challenges states will face in implementing the provision for youth formerly in foster care is keeping them aware of their categorical eligibility. Youth who lose Medicaid eligibility under other criteria or who lose a job that had provided health insurance benefits remain eligible for Medicaid as former foster youth until they turn 26 years old. Similarly, youth who leave the military or prison retain Medicaid eligibility if they left foster care after their 18th birthday and are under 26. In addition to being eligible for Medicaid, youth who age out of foster care are eligible for a comprehensive benefits package probably not available to other comparably aged youth. States need to develop systems that identify youth as formerly in foster care or find ways to keep youth informed of their rights when no longer involved with the child welfare system.
In addition, service providers for youth should be made aware of the provision on coverage for youth who have aged out of care, so they may think about whether the coverage is pertinent for the individuals they serve. For example, those who work with young adults leaving the justice system may not be aware of the young person’s eligibility for Medicaid. Similarly mental health providers and substance abuse service providers may deal with former foster youth without realizing that the young people are eligible for coverage. Providing information and training to workers in these systems may help reconnect youth who have fallen out of the Medicaid system.
Finally, the Affordable Care Act provision represents a national requirement to provide Medicaid coverage to youth who age out of foster care. However, the child welfare system is managed within each state and no system exists for one state to know if a young person had been in foster care in another state. Whether states can coordinate in a way that prevents these youth from falling through the cracks is an open question.
REFERENCES
Baumrucker, E. P., A. L. Fernandes-Alcantara, E. Stoltzfus, and B. Fernandez. 2012. “Child Welfare: Health Care Needs of Children in Foster Care and Related Federal Issues.” Washington, DC: Congressional Research Service.
Collins, S., and J. Nicholson. 2010. “Rite of Passage: Young Adults and the Affordable Care Act of 2010.” New York: The Commonwealth Fund.
Courtney, M. E., and A. Dworsky. 2006. “Midwest Evaluation of the Adult Functioning of Former Foster Youth from Iowa: Outcomes at Age 19.” Chicago: Chapin Hall Center for Children at the University of Chicago.
Courtney, M. E., A. Dworsky, A. Brown, C. Cary, K. Love, and V. Vorhies. 2011. “Midwest Evaluation of the Adult Functioning of Former Foster Youth: Outcomes at Age 26.” Chicago: Chapin Hall at the University of Chicago.
Courtney, M. E., A. Dworsky, G. R. Cusick, J. Havlicek, A. Perez, and T. Keller. 2007. “Midwest Evaluation of the Adult Functioning of Former Foster Youth: Outcomes at Age 21.” Chicago: Chapin Hall at the University of Chicago.
Courtney, M. E., A. Dworsky, J. Lee, and M. Raap. 2010. “Midwest Evaluation of the Adult Functioning of Former Foster Youth: Outcomes at Age 23 and 24.” Chicago: Chapin Hall Center at the University of Chicago.
Courtney, M. E., A. Dworsky, G. Ruth, T. Keller, J. Havlicek, and N. Bost. 2005. “Midwest Evaluation of the Adult Functioning of Former Foster Youth: Outcomes at Age 19.” Chicago: Chapin Hall Center for Children at the University of Chicago.
Dorn, S. 2007. “Eligible but Not Enrolled: How SCHIP Reauthorization Can Help.” Washington, DC: The Urban Institute. http://www.urban.org/publications/411549.html.
Dorn, S., I. Hill, and S. Hogan. 2009. “The Secrets of Massachusetts’ Success: Why 97 Percent of State Residents Have Health Coverage.” State Health Access Reform Evaluation. Washington, DC: The Urban Institute. http://www.urban.org/publications/411987.html.
English, A. 2006. “Youth Leaving Foster Care and Homeless Youth: Ensuring Access to Health Care.” Temple Law Review 79:439–59.
Goerge, R. L., B. Bilaver, B. Joo Lee, A. Needell, A. Brookhart, and W. Jackman. 2002. “Employment Outcomes for Youth Aging Out of Foster Care.” Chicago: Chapin Hall Center for Children at the University of Chicago.
Hanna, T., A. Radican-Wald, and W. Prater. 2008. “A Profile of Children’s Health Coverage in Mississippi.” Jackson: Center for Mississippi Health Policy.
Hill, I., and A. Westpfahl Lutzky. 2003. Getting In, Not Getting In, and Why: Understanding SCHIP Enrollment. Washington, DC: The Urban Institute. Assessing the New Federalism Occasional Paper 66. http://www.urban.org/publications/310793.html.
Howell, E. M., Palmer, A., and Adams, F. 2012. “Medicaid and CHIP Risk-Based Managed Care in 20 States: Experiences over the Past Decade and Lessons for the Future.” Final Report to the Office of the Assistant Secretary for Planning and Evaluation, U.S. Department of Health and Human Services. Washington, DC: The Urban Institute.
http://www.urban.org/publications/412617.html.
Kaiser Family Foundation 2012. “Summary of New Health Reform Law.”
http://www.kff.org/healthreform/upload/8061.pdf. (Accessed August 23, 2012.)
Kenney, G., and J. Haley. 2001. “Why Aren’t More Uninsured Children Enrolled in Medicaid or SCHIP?” Washington, DC: The Urban Institute. Assessing the New Federalism Policy Brief B-35. http://www.urban.org/publications/310217.html.
Kenney, G., A. Cook, and L. Dubay. 2009. “Progress Enrolling Children in Medicaid/CHIP: Who Is Left and What Are the Prospects for Covering More Children?” Timely Analysis of Immediate Health Policy Issues. Washington, DC: The Urban Institute.
http://www.urban.org/publications/411981.html.
Kenney, G., J. Pelletier, and L. Blumberg. 2010. “How Will the Patient Protection and Affordable Care Act of 2010 Affect Young Adults?” Timely Analysis of Immediate Health Policy Issues. Washington, DC: The Urban Institute. http://www.urban.org/publications/412130.html.
Lewis, N. 2008. Memo to ACCESS Florida Operations Managers, TRANSMITTAL C – 08-08-0011. Tampa, FL: Center for Child Welfare. http://centerforchildwelfare2.fmhi.usf.edu/kb/policymemos/08_08_01_MedicaidFormerFY_ACCESS.pdf
Patel, S., and M. A. Roherty. 2007. “Medicaid Access for Youth Aging Out of Foster Care.” Washington, DC: American Public Human Services Association.
Pecora, P. J., R. C. Kessler, J. Williams, A. C. Downs, D. English, J. White, C. Roller White, T. Wiggins, and K. Holmes. 2005. “Improving Family Foster Care: Findings from the Northwest Alumni Study.” Seattle, WA: Casey Family Programs.
Pergamit, M. R., V. Chen, M. McDaniel, and E. Howell. 2012. “Assessing the Impact of Differences in Implementation of the Chafee Medicaid Option on Medicaid Coverage for Youth Who Age Out of Foster Care.” Unpublished manuscript, The Urban Institute, Washington, DC. available from the authors.
Perry, M., and A. Betty. 2010. “Consumer Voices: What Motivates Families to Enroll in Coverage?” Presented at the CMS webinar session “CHIP and Medicaid Enrollment through Effective Messaging,” Washington, DC, September 14.
Schwartz, S., and M. Glascock. 2008. “Improving Access to Health Coverage for Transitional Youth.” Washington, DC: The National Academy for State Health Policy.
———. 2011. The AFCARS Report: Preliminary FY 2010 Estimates as of June 2011 (18).Washington, DC: U.S. DHHS.http://www.acf.hhs.gov/programs/cb/stats_research/afcars/tar/report18.htm.
APPENDIX A: Study Methodology
Data for this report came from three primary sources: published documentation from reports and web sites, direct discussions with state administrators and staff and other knowledgeable informants, and analysis of Medicaid enrollment and claims and encounter records collected by states as part of their routine administration of the Medicaid program.
Reports and Web Sites
We consulted several reports and web sites from national and state agencies and organizations to gather published information on states’ implementations of the Chafee Option (for example, Dworsky and Havlicek 2009; Irvin and Brown 2008; http://www.nrcyd.ou.edu/, 2010). From these sources we were able to determine which states had taken the Chafee Option14 and collect information on eligibility criteria, general enrollment procedures, and redetermination rules.
General Sources
Casey Family Programs. 2007. “The Chafee Educational and Training Voucher Program.” National Foster Care Coalition. http://www.casey.org/Resources/Publications/pdf/ChafeeETV.pdf.
Dworsky, A., and J. Havlicek. 2009. “Review of State Policies and Programs to Support Young People Transitioning Out of Foster Care.” Chicago: University of Chicago, Chapin Hall Center for Children.
Irvin, C., and J. Brown. 2008. “Examining States’ Experiences Providing Medicaid to Youth Aging Out of Foster Care.” Washington, DC: Office of the Assistant Secretary for Planning and Evaluation, Department of Health and Human Services.
Mockingbird Society. 2007. “Chafee by State.” http://www.mockingbirdsociety.org.
National Child Welfare Resource Center for Youth Development and the National Foster Care Coalition. 2009. “State by State Fact Pages.” http://www.nrcyd.ou.edu/state-pages.
Patel, S., and M. A. Roherty. 2007. “Medicaid Access for Youth Aging Out of Foster Care.” Washington, DC: American Public Human Services Association.
State Government Sources
ACCCHS. 2011. “Health Insurance for Children.” State of Arizona Medicaid Agency.
http://www.azahcccs.gov/applicants/categories/children.aspx.
Arizona Department of Economic Security. “Independent Living/Young Adult Program: Physical and Mental Health.” https://www.azdes.gov/main.aspx?menu=150&id=1786.
Colorado Division of Child Welfare. “Chafee Foster Care Independence Program.” Colorado Department of Human Services.
http://www.colorado.gov/cs/Satellite/CDHS-ChildYouthFam/CBON/1251589743194.
Colorado General Assembly. 2007. “Digest of Bills 2007: Health Care Policy and Financing.” http://www.state.co.us/gov_dir/leg_dir/olls/digest2007a/HEALTHCAREPOLICY....
———. 2008. “Digest of Bills 2008: Health Care Policy and Financing.”
http://www.state.co.us/gov_dir/leg_dir/olls/digest2008a/HEALTHCAREPOLICY....
Connecticut Department of Children and Families. 2007. “Title XIX Medical Coverage: Terminating/Transitioning Medical Coverage.” Chapter 16-4-4. http://www.ct.gov/dcf/cwp/view.asp?a=2639&Q=390552.
Delaware Department of Services for Children, Youth, and Their Families. 2010. “Memorandum of Understanding among Delaware State Agencies Regarding Aging Out of Foster Care Children.” State of Delaware. http://kids.delaware.gov/pdfs/mou_AgingOut.pdf.
Georgia Independent Living Program. “Chafee Medicaid.” Georgia Department of Human Services.
http://www.georgiailp.org/supported_services.php
Independence for Foster Youth. 2010. “Medicaid to 21.” State of Washington. http://www.independence.wa.gov/programs/medicaid21.asp.
Indiana Department of Child Services. 2006. “Independent Living Service Timeline.” http://www.in.gov/dcs/files/ilbullaugsept2006.pdf, page 4.
Just for Youth. “A Guide to Medicaid after Leaving Foster Care: For the 18–21-Year-Old Already Covered by Medicaid.” Utah Department of Human Services. http://health.utah.gov/umb/forms/pdf/fc_il.pdf.
Kansas Department of Children and Family Services. 2011. “7221: Eligibility for Foster Care Medical Card Extension Program.” CFS-Policy and Procedure Manual. http://content.srs.ks.gov/cfs/robohelp/ppmgenerate /7000/7221_Eligibility_for_Foster_Care_Medical_Card_Extension_Program.htm
Kansas Department of Children and Family Services. 2011. “7910 Independent Living Medical Card Extension Program Procedures.” CFS-Policy and Procedure Manual. http://content.dcf.ks.gov/PPS/robohelp/PPMGenerate/7000_Independent_Livi....
Kansas Department of Social and Rehabilitation Services. 2010. “Comprehensive Child and Family Services State Plan: FY 2010–2014.” Annual Progress and Services Report. http://www.dcf.ks.gov/services/PPS/Documents/Other/ComprehensiveCFSstate....
Louisiana State Senate. 2008. “Medicaid: Session 2008 Highlights.” http://senate.legis.state.la.us/sessioninfo/2008/.
Massachusetts Department of Children and Families. “Chafee Foster Care Independence Program and Education and Training Voucher Program.”http://www.mass.gov/eohhs/docs/dcf/program-report-chafee-and-etv.pdf.
Medi-Cal Handbook. 2010. “22.5 Extended Medi-Cal Eligibility for Former Foster Care Children.” In “22. Continued Eligibility for Pregnant Women, Infants, and Children.” http://www.sccgov.org/ssa/medical/mcchap22.pdf.
Michigan Department of Human Services. 2001. “John H. Chafee Foster Care Independence Program: Michigan FY 2001–2004 Application Outline.” http://www.michigan.gov/documents/FIA-Chafee-FosterCarePlanFY2001-2004_1....
———. 2008. “Foster Care Transitional Medicaid.” http://www.michigan.gov/documents/dhs/DHS-PUB-0193_263806_7.pdf.
Missouri Children’s Division. 2008. “Chafee Foster Care Independent Living Services Program (CFCIP).” Missouri Department of Social Services. http://www.dss.mo.gov/cd/cfsplan08/pdf/sec11.pdf.
Missouri Children’s Division. 2009. “Aftercare Program.” Missouri Department of Social Services. http://www.dss.mo.gov/cd/chafee/aftercare.htm.
Nevada Division of Child and Family Services. 2007. “Independent Living Program.” Department of Health and Human Services. http://www.dcfs.state.nv.us/DCFS_IndependentLiving.htm.
North Carolina Department of Social Services. 2010. “Helping Teens Make a Successful Transition from Foster Care to Self-Sufficiency.” http://www.ncdhhs.gov/dss/links/.
Ohio Department of Jobs and Families. “Medicaid Program Overview.” http://www.jfs.ohio.gov/OHP/bcps/FactSheets/Medicaid.pdf.
Oregon State Legislature. 2010. “75th Oregon Legislative Assembly: 2010 Special Session—House Bill 3664.” http://www.leg.state.or.us/10ss1/measures/hb3600.dir/hb3664.intro.html.
Rhode Island Department of Children, Youth, and Families. 2008. “Services to Youth Ages 18–21.” Policy: 700.0240. http://www.dcyf.ri.gov/docs/services_to_youtp8_21.pdf.
South Carolina Department of Social Services. “Foster Care Services.” https://dss.sc.gov/content/customers/protection/fcs/index.aspx.
South Dakota Department of Social Services, Medical Eligibility, Families and Children. 2011. “Medical Assistance for Youth Formerly in Foster Care.” http://dss.sd.gov/medicaleligibility/familieschildren/formerfostercare.asp.
Tennessee Youth Advisory Council. “Department of Children's Services.” http://www.state.tn.us/youth/.
Texas Department of Family and Protective Services. 2010a. “State- and Federally-Funded Programs for Individuals Currently or Formerly in Foster Care.” Transitional Living Services.
http://www.dfps.state.tx.us/Documents/Child_Protection/pdf/transitionalmedicaid.pdf
———. 2010b. “Transitional Living Services.”
http://www.dfps.state.tx.us/Child_Protection/Transitional_Living/.
Utah State Legislature. H.B. 288: Health Care Amendments for Foster Children.
Wisconsin Division of Safety and Permanence. 2008. “DSP INFO MEMO 2008—01.” Division of Children and Families: State of Wisconsin. http://dcf.wisconsin.gov/memos/num_memos/2008/2008-03.pdf.
Wyoming Department of Family Services. 2009. Chapter 14: IV-E Foster Care Policy Manual. Policy Number: IV-E 09-003. (Revised 7/1/11 as Policy Number IV-E-001 and available at
https://docs.google.com/a/wyo.gov/file/d/0B-2EkWB4ILAQaUpwSUg2TEVhNjQ/edit?pli=1)
State Advocacy Sources or Other Third-Party, State-Specific Sources
Florida's Children First, Inc. 2007. “FAQ for Foster Youth Transitioning to Adulthood.” http://www.FloridasChildrenFirst.org.
Iowa After Care. 2008. “Options for Iowa Foster Youth as They Reach Age 18.” Youth Policy Institute of Iowa. http://www.iowaaftercare.org/options_at_18.pdf.
Justia US Law. 2009. 2009 “Louisiana Code Title 46:: RS46:450.6 Election of Chafee Option.” http://law.justia.com/louisiana/codes/2009/rs/title46/rs46-450.6.html.
National Law Health Program. 2008. “Medi-Cal for Children Turning Age 18 while in Foster Care.” Health Consumer Alliance. http://www.healthconsumer.org/cs036Fostercare.pdf.
New Jersey Alliance for Children, Youth, and Families. “Services for Youth Aging Out of the Child Welfare System.” http://www.njacyf.org/Resources/Aging-Out.asp.
Wagner, J. O., and M. E. Wonacott. 2008. “Youth Aging Out of Foster Care.” Learning Work Connection. Sponsored by Ohio Department of Job and Family Services, Office of Workforce Development, Bureau of Workforce Services. http://cle.osu.edu/lwc-publications/youth-information-briefs/downloads/Y....
Discussions with State Officials and Others
Published documents did not include all the information we needed to fully understand how the Chafee Option was implemented in each state. Information, such as how implementation varied across the state (e.g., whether procedures were standard or varied by jurisdiction), whether any procedures have changed since the Chafee Option was enacted, and implementation experiences and interagency collaborations was not documented. Also, material we found on each state was not always complete or current. For example, exact implementation dates were readily found for some states but not others. After collecting as much information as we could find, we created detailed grids of the information we had for each state and identified categories where more information was needed. We customized a set of questions for each state based on these grids. Sample discussion topics included
- Chafee Option implementation rules and procedures
- What are eligibility requirements and restrictions?
- What are the application procedures —how do youth apply?
- Does a caseworker handle the bulk of the application procedures?
- What are the rules for redetermination?
- Chafee Option implementation experiences
- When was the Chafee Option implemented?
- How long did implementation take?
- Who were the parties involved in implementation?
- Have there been any significant changes since implementation? If so, what were they and why?
- Child welfare/Medicaid agency relationship and collaboration
- What are the respective roles and responsibilities of the child welfare and Medicaid agencies?
- How would you describe the relationship between the child welfare and Medicaid agencies?
- What are some lessons you/your agency learned in implementing the Chafee Option?
Using the customized set of questions for each state, we contacted the state’s independent living coordinator, who is the program lead for services to youth currently and formerly in foster care, and scheduled a time to talk by telephone. In most cases our discussions were with the state’s independent living coordinator; in many cases coordinators were joined by a representative from either the Medicaid agency or a Medicaid liaison within the child welfare agency. In most cases we spoke with one or two people. In a few states we did not speak to the independent living coordinator but to someone to whom he or she referred us who was more knowledgeable about Chafee Option procedures and implementation. Discussions took place during the winter and spring of 2011. Table A.1 shows counts of the types of people we spoke with in the 30 states.
TABLE A.1: Key Informants in the 30 Chafee Option States
| Position | Number |
|---|---|
| State Independent Living Coordinator | 24 |
| Child Welfare Agency Medicaid Specialist | 3 |
| Child Welfare Agency Program and Policy Administrator | 12 |
| Medicaid Agency Eligibility and Policy Specialist | 14 |
| State Advocacy/Social Service Organization | 3 |
| TOTAL | 56 |
Medicaid Statistical Information System Data
Data used for the quantitative analysis come from the Medicaid enrollment and claims/encounter records collected by states as part of their routine administration of the Medicaid program. Since 1999, states have been required to submit quarterly—as part of the Medicaid Statistical Information System (MSIS)—a uniform extract of these records to the Centers for Medicare and Medicaid Services. States must submit monthly records of whether each person was enrolled in a given month and the eligibility group for which they qualified.
We use the MSIS Annual Summary File which includes person-level data on Medicaid eligibility and expenditures by type of services, as well as demographic and managed care participation. This MSIS extract is prepared annually, once data are received from states and includes all claims paid in a year on a federal fiscal year basis. Youth were identified as being in foster care in the month preceding their 18th birthday (age 17 years, 11 months)15 in FY2006. Annual files from FY2006, FY2007, and FY2008 were linked so we could follow these youth for two years.
The sample includes youth from 10 of the 30 states that implemented the Chafee Option. Three criteria determined the states included in the analysis. First, the state had to have implemented the Chafee Option by FY2006 in order to allow us to observe enrollment in three consecutive fiscal years.16 Seventeen states met this criterion. Second, a state-specific code had to be available to distinguish youth in foster care from adopted youth. These codes were not available for an additional three states. Third, the state had to provide adequate sample sizes for analysis. This criterion was applied at two points. Two of the remaining states were excluded for having fewer than 400 youth emancipating from foster care in FY2006 based on data from the Adoption and Foster Care Administrative Reporting System and an additional 2 states were excluded for having fewer than 100 17-year-old youth in the MSIS data in FY2006. The 10 states that met all three criteria are included in the analysis: Arizona, Kansas, Utah, California, Florida, Indiana, Iowa, Nevada, South Carolina, and Texas.
In total, we identified 9,662 youth age 17 years, 11 months, in foster care in these 10 states in FY2006.17 For the analysis of service use, we limit the sample to a subset of youth. Although enrollment records for these youth should be complete, states that enroll foster youth or former foster youth in managed care will not have complete records for service use because most managed care organizations are not paid based on claims/encounters. For analysis of service use, we exclude youth enrolled in managed care plans available in three states (Arizona, Iowa, and Nevada) and in some counties in California, Florida, Indiana, and Utah. This restriction results in 7,565 youth in the sample for examining service use.
APPENDIX B: Age-Out Policies by State
| State | Maximum Agea | Brief Descriptionb |
|---|---|---|
| Arizona | 21 | Youth may remain in care to age 21 under a voluntary agreement. Youth who leave care at age 18 or older may return to care at any time before their 21st birthday. |
| California | 18 | Youth can stay in care past their 18th birthday if they intend to graduate from high school before their 19th birthday. |
| Colorado | 21 | Youth can stay in care “under special circumstances.” Examples of special circumstances are mental illnesses, developmental issues, or pursuing postsecondary education. The choice to stay in care is one that is made in the best interest of the youth and happens among the court, county department, guardian ad litem, youth, caseworker, and administrator. |
| Connecticut | 23 | Anyone committed to the Department of Children and Families prior to their 18th birthday is eligible for D04 services for transitioning out of care. They must reside in Connecticut. Youth can decline services and still be eligible for the program with some modifications. |
| Florida | 18 | Young adults may request an extension of jurisdiction until age19 so that they can complete high school. The court may also retain jurisdiction beyond a youth’s 18th birthday under special circumstances determined by the court (e.g., extended jurisdiction for youth awaiting decision on their immigration status). The jurisdiction terminates upon the final decision by the federal authorities or when the young adult turns 22, whichever is earlier.
|
| Georgia | 21 | Youth may remain in care through age 21 if they have an educational plan and sign an agreement with the resource provider and the county. Youth may remain in care until 21.5 years if the additional six months will allow time to complete an educational program. |
| Indiana | 21 | Youth in high school and making a concerted effort to graduate may be maintained in care by the courts beyond age 18. Youth waiting for adult services, such as disability services, may also stay in care past 18. |
| Iowa | 20 | Youth can stay in care until age 20 as long as they are pursuing a GED or high school diploma. |
| Kansas | 21 | Youth need a transition plan. Youth who want to stay in care beyond their 18th birthday must have a court approved transition plan that demonstrates the need to stay in care. Youth have always been able to stay in care until age 21; however few stay in care past age 18. |
| Louisiana | 18 | There is no formal extension of care, but youth may enter a “voluntary contract between the ages of 18–21 to receive ongoing case management and financial support for housing if they are in a vocational or educational program or are working and taking classes full time. This includes postsecondary education, a GED, or a high school diploma. Payments to the caregiver or for independent living will continue. Regardless of the contract, any former foster youth may contact a caseworker to ask questions without any associated costs. Caseworkers can continue to act as a resource for youth up to age 21. |
| Maryland | 21 | Youth can remain in care if they are working, attending school or a vocational program, or are disabled. In 2010, the State developed a new policy that allows foster youth who leave care after age 18 to return to care. |
| Massachusetts | 22 | Youth can sign a voluntary placement agreement with the Department of Children and Families when they turn 18 if they are willing to continue pursuing their education or vocational training (including postsecondary education) and comply with their service plan. They may also stay in care longer if they are applying for adult services such as mental health or disability services. |
| Michigan | 21 | Youth can sign a voluntary agreement to continue to receive services if meet Fostering Connections requirements. At time of this writing, at each county’s discretion, foster youth could continue foster care payments if they have reached age 19 and were still in a school or training program. |
| Mississippi | 21 | Youth may remain in care until age 21 under a court order. |
| Missouri | 21 | Youth may remain in care if they are in school, have a court order, or if it is in their best interest. The juvenile judge has ultimate authority regarding whether a youth remains in care. |
continued
| State | Maximum Agea | Brief Descriptionb |
|---|---|---|
| Nevada | 21 | Youth are not officially in foster care past 18 but may sign a voluntary agreement and then continue receiving the same care and opportunities as though they were in foster care. They must be enrolled in an authorized school or education program (for secondary or equivalent training) or be completing a high school diploma or GED and making satisfactory progress. They may not run away. |
| New Jersey | 21 | Youth may remain in care if they have not graduated from high school or if they need special treatment that cannot be provided otherwise. |
| New Mexico | 18 | Beyond 18, youth can continue to receive services but are not in foster care. The court can maintain jurisdiction to monitor their progress to age 19; however, this is voluntary on the youth’s part. |
| North Carolina | 18 | Youth may sign a voluntary contractual agreement for residential services upon their 18th birthday. The extended care does not involve the court. The youth must be continuing education (high school or post-secondary) or be engaged in a vocational training program. This service is available for youth that had been in legal custody for some time prior to, but not necessarily on, their 18th birthday. |
| Ohio | 18 | Youth may stay in care until age 19 to finish high school or for certain medical reasons. |
| Oklahoma | 21 | Youth are allowed to remain in placement and receive voluntary services after age 18 if they have not completed high school or a GED. Also youth must have been in an out-of-home placement on their 18th birthday to qualify for Medicaid under the Chafee Option. |
| Oregon | 21 | Youth may remain in care if they are completing high school or a GED, or have an individualized education plan. Exceptions are also available if reviewed and approved by the branch manager. |
| Rhode Island | 18 | All youth in the care and custody of the Department for reasons other than juvenile delinquency are terminated by the Family Court upon reaching the age of 18. The Department will keep open and continue to provide services, up to age 21, to youth identified as seriously emotionally disturbed or have a functional developmental disability, and not yet eligible for the adult system of care. Other former foster care youth who leave the Department on or after their 18th birthday are closed by the Department but may be eligible for Aftercare Support Services provided through private agencies. They must apply for such services. These services provide limited management supports, the establishment of budget/living expenses and some assistance with such expenses, and the establishment of a self-sufficiency plan. |
| South Carolina | 21 | In keeping with Fostering Connections, youth may stay in care if they are employed or pursuing their education (secondary or postsecondary), are in vocational training, or are in an activity that could lead to employment (e.g., volunteer work). |
| South Dakota | 21 | Youth may stay in care until age 21 if they have not completed high school. |
| Texas | 22 | Youth may stay in foster care by signing a voluntary extended foster care agreement. Remaining in foster care allows the youth to • finish high school (up to the month of their 22nd birthday) or a GED program; • attend college or other postsecondary educational or vocational activities; • obtain employment or enhance work-related skills and knowledge through employment readiness activities; and • if applicable, eligibility may be established for youth incapable of performing the activities described above due to a documented medical condition. Under the Return to Care program, implemented in September 2007, certain eligible youth who aged out of care can return to care until age 21 to attend a vocational or technical program or take a short break from college or a vocational or technical program for at least one month but no more than four months or until age 22 to attend high school or a GED program. With the passage of state legislation, beginning September 28, 2011, youth may return from a trial independence period to start or resume extended foster care. |
| Utah | 21 | Youth may remain in jurisdiction until age 21 if they are completing high school and have plans to live in the community. The court decides who may remain in jurisdiction. |
continued
| State | Maximum Agea | Brief Descriptionb |
|---|---|---|
| a. Maximum age refers to the maximum age that youth may typically stay in care. b. The brief descriptions include information from official documentation and conversations with knowledgeable staff about the process. | ||
| Washington | 21 | Beginning July 22, 2011, youth needing to complete high school or obtain their GED may elect to participate in extended foster care, which requires a continuation of the dependency petition until they graduate from high school, obtain their GED, or turn 21, whichever comes first. There is a six month “grace period” for youth who initially opt out of extended foster care services at age 18 and then later decide to participate. Youth may also apply for “Foster Care to 21” for postsecondary education, but this is not available to everyone. Foster Care to 21 went into effect in 2006. |
| Wisconsin | 19 | Youth may stay in care until age 19 to finish high school, or a GED, or to get a diploma as long as the youth are expected to graduate at the end of the year. If they are more than one years’ worth of credits behind, there is no extension. |
| Wyoming | 21 | Most youth who stay in care until 21 are those in a facility, have an individualized education plan, need specialized education until age 21, or receive Board of Cooperative Education Services. Many of these youth receive SSI and may require more time to fulfill education requirements. |
APPENDIX C: Eligibility Criteria by State
| State | Brief Description |
|---|---|
| a. Supplemental Security Income. | |
| INCOME AND RESOURCE REQUIREMENTS | |
| Indiana | Less than 200% of the federal poverty level |
| Iowa | Less than 200% of the federal poverty level |
| Maryland | Less than 300% of the federal poverty level |
| Oklahoma | Less than 180% of the federal poverty level |
| Texas | Less than 400% of the federal poverty level; less than, $10,000 in assets |
| STATES ALLOWING YOUTH FROM OTHER STATES | |
| Georgia | Youth who were in foster care in a different state at age 18 are eligible |
| Louisiana | Youth who were in foster care in a different state at age 18 are eligible |
| Texas | Youth who were in foster care in a different state at age 18 are eligible |
| Wisconsin | Youth who were in foster care in a different state at age 18 are eligible |
| SCREENING FOR OTHER MEDICAID ELIGIBILITY | |
| Arizona | Youth are screened for eligibility under other Medicaid coverage groups first |
| California | Youth who are disabled will be enrolled for Medicaid under SSI,a not Chafee |
| Colorado | Youth who are disabled will be enrolled for Medicaid under SSI, not Chafee |
| Connecticut | Youth who are disabled will be enrolled for Medicaid under SSI, not Chafee |
| Florida | Youth who are disabled will be enrolled for Medicaid under SSI, not Chafee |
| Georgia | Youth who are disabled will be enrolled for Medicaid under SSI, not Chafee |
| Indiana | Youth who are disabled will be enrolled for Medicaid under SSI, not Chafee |
| Iowa | Youth who are eligible under other Medicaid coverage groups can be enrolled in Medicaid under the Chafee Option unless the youth is a mandatory household member under another coverage group. |
| Kansas | Youth are screened for eligibility for other Medicaid coverage groups first |
| Louisiana | Youth who are disabled will be enrolled for Medicaid under SSI, not Chafee |
| Maryland | Youth are screened for eligibility for other Medicaid coverage groups first |
| Mississippi | Youth who are disabled will be enrolled for Medicaid under SSI, not Chafee |
| Missouri | Youth are screened for eligibility for other Medicaid coverage groups first |
| Nevada | Youth are screened for eligibility for other Medicaid coverage groups first |
| New Jersey | Youth are screened for eligibility for other Medicaid coverage groups first |
| New Mexico | Youth who are disabled will be enrolled for Medicaid under SSI, not Chafee; also, youth who are pregnant are likely to be enrolled in Medicaid based on their pregnancy. |
| North Carolina | Youth are screened for eligibility for other Medicaid coverage groups first |
| Ohio | Youth who are disabled will be enrolled for Medicaid under SSI, not Chafee |
| Oklahoma | Youth are screened for eligibility for other Medicaid coverage groups first |
| Oregon | Youth who are disabled will be enrolled for Medicaid under SSI, not Chafee |
| Rhode Island | Youth who are disabled will be enrolled for Medicaid under SSI, not Chafee |
| South Carolina | Youth who are disabled will be enrolled for Medicaid under SSI, not Chafee |
| Texas | Youth are screened for eligibility for other Medicaid coverage groups first |
| Utah | Youth are screened for eligibility for other Medicaid coverage groups first |
| Washington | Youth who are disabled will be enrolled for Medicaid under SSI, not Chafee |
| Wisconsin | Youth who are disabled will be enrolled for Medicaid under SSI, not Chafee |
| Wyoming | Youth who are disabled will be enrolled for Medicaid under SSI, not Chafee |
APPENDIX D: Enrollment Process by State
|
| State | Applicationa |
Brief Descriptionb | ||||
|---|---|---|---|---|---|---|---|
| None | Tailored | Standard | |||||
| YOUTH IS NOT DIRECTLY INVOLVED IN ENROLLMENT PROCESS | |||||||
| Complete Automation | Louisiana | X |
|
| Medicaid is “automatically sustained.” Child welfare and Medicaid data systems interface, and youth remain covered by Medicaid until age 21, unless Medicaid receives an alert to close the case. | ||
| Missouri | X |
|
| When the foster care case closes, the system automatically triggers a process that allows enrollment in Medicaid under the Chafee Option and allows youths’ information to be transferred to the Medicaid system. | |||
| Automatic Alert to Medicaid when Case Closed | California | X |
|
| When youth age out, a Medi-Cal worker will check their’ eligibility and then continue their Medicaid coverage. The youth are already in the Medi-Cal system. Medi-Cal will then send the youth a confirmation enrollment letter. | ||
| Florida | X |
|
| When youth age out, an electronic alert is activated in the data system; child welfare revenue maximization specialists work with case managers (and youth) to acquire eligibility information (e.g., current address). The information is sent electronically to Florida’s ACCESS office (which determines eligibility for services including Medicaid, food stamps, and cash assistance). | |||
| Michigan | X |
|
| The current system (since early 2010) involves automatic enrollment. A special system code will automatically indicate a youth’s eligibility for Medicaid under the Chafee Option. An enrollment packet will be mailed to the youth, who may choose a plan and sign up. | |||
| Texas | X |
|
| The child welfare and Medicaid electronic systems are interfaced. When a youth ages out, a caseworker will send an automatic referral to the Medicaid system. If the referral fails, the youth may also fill out an application. | |||
| Washington | X |
|
| When the youth has left care, the child welfare system alerts the Medicaid system, which will change the youth’s Medicaid eligibility code. A foster care Medicaid unit is responsible for verifying that the youth is eligible. | |||
| Automatic Alert to Child Welfare, Who Notifies Medicaid or Enrolls on Own | Colorado | X |
|
| County staff are alerted to switch youth into Medicaid under the Chafee Option through the Medicaid system. Youth are given ID and Medicaid cards. | ||
| Massachusetts | X |
|
| The child welfare system’s information technology group is alerted when youth age out; they verify eligibility and send the name and information to Mass Health. | |||
| Rhode Island | X |
|
| Child welfare staff view automated reports of status changes and make appropriate updates to reflect the changes in the state Medicaid database. | |||
continued
|
| State | Applicationa | Brief Descriptionb | ||
|---|---|---|---|---|---|
| None | Tailored | Standard | |||
| YOUTH IS NOT DIRECTLY INVOLVED IN ENROLLMENT PROCESS (continued) | |||||
| Automatic Alert to Child Welfare, Who Notifies Medicaid or Enrolls on Own (continued) | South Carolina | X |
|
| Youths’ case managers will inform Medicaid informally that they will be continuing on Medicaid. Youth do not need to do anything, and there is no formal application. |
| South Dakota | X |
|
| A monthly report that contains information on exiting youth automatically alerts the independent living coordinator and Medicaid contact, who then switch the youth to Medicaid under the Chafee Option in their data system. | |
| Caseworker Fills Out Application for Youth and Sends to Medicaid | Indiana |
| X |
| A Medicaid eligibility worker is alerted by a flag indicating that a youth is turning 18. The case manager fills out the paperwork and sends it to Medicaid. |
| Iowa | X |
|
| A caseworker will send the youth’s case information to a Medicaid worker, who will verify eligibility and enroll the youth. The youth does not need to be present. | |
| Mississippi | X |
|
| Once the youth leaves care, child welfare services fills out a form to stop foster care Medicaid. The Division of Medicaid will automatically transfer coverage to Medicaid under the Chafee Option if the child is over 18. | |
| YOUTH IS INVOLVED IN ENROLLMENT WITH CASEWORKER ASSISTANCE | |||||
| Youth Works with Caseworker and Has Minimal Role | Connecticut |
| X |
| The youth’s caseworker fills out an application for Medicaid with the youth. The information is sent to the Medicaid eligibility group in the child welfare office, which will forward the information to Medicaid using a different form. |
| New Mexico |
| X |
| A worker ideally helps the youth fill out a form (name, address, date of birth, social security number, marital status, history of felonies, income), teaching him or her how to make an appointment, get medication refills, and address any other medically related questions. | |
| Oregon |
| X |
| The caseworker completes a one-page application with youth, which is sent to a federal revenue specialist, who verifies the youth’s eligibility. Medicaid sends a packet to the youth at the specified mailing address that must be deliverable (i.e., not returned). The youth does not need to respond or return anything. | |
| New Jersey | X |
|
| As part of the youth's transition plan, the caseworker makes a referral with the youth or on behalf of the youth. Youth ages 18–20 who are not already enrolled may also call a hotline number to get enrolled any time after their 18th birthday. | |
| Youth Must Sign Application | Arizona |
| X |
| A caseworker sits with the youth to fill out an application that is sent to the Family Assistance Administration (FAA). Youth choose a health plan and their signature is necessary. Youth can also apply at a local FAA office if coverage lapses or they are not available to pre-enroll at age 18. Currently, the Arizona Medicaid application includes a question regarding foster care status at age 18 to assist in identifying eligible applicants. |
continued
|
| State | Applicationa | Brief Descriptionb | ||
|---|---|---|---|---|---|
| None | Tailored | Standard | |||
| YOUTH IS INVOLVED IN ENROLLMENT WITH CASEWORKER ASSISTANCE (continued) | |||||
| Youth Must Sign Application (continued) | Georgia | X |
|
| Independent living staff notify foster care Medicaid eligibility workers in the month prior to a youth aging out; Eligibility workers will check eligibility and enroll the youth. If this does not occur, the youth can go to a county Department of Family and Children Services office and apply for Medicaid and check a box for former foster youth. They must sign a third-party rights form to be enrolled. |
| Kansas |
| X |
| As part of transition plan, the caseworker will make sure that an application is filled out, which is given to the independent living worker, who obtains the youth’s signature and submits it for processing to regional staff. Youth need to show citizenship or special juvenile immigration status, but typically this information is already available. | |
| Nevada |
| X |
| Caseworkers help youth fill out the application during their transition planning (at least 90 days before the youth leaves care) and submit the application to the Medicaid office. Each county varies slightly in the amount of paperwork required and what documents must be provided. | |
| Ohio |
| X |
| Youth must take the initiative to fill out three forms, with the help of a caseworker, who sends the forms to Jobs and Family Services. If the youth do not get enrolled in this manner, they can contact the Public Children’s Service Association to get enrolled. | |
| Oklahoma |
|
| X | Youth fill out a Medicaid application that they must sign during their child welfare exit interviews. The application is then sent to a central person at the Medicaid office, who will enroll youth for one year. Before 2011, youth would enroll on their own at the Medicaid office. | |
| Youth Must Provide or Return Additional Documentation | Utah |
|
| X | Youth and their caseworkers complete during the 90-day transition plan an application, which the youth must sign. The application is submitted to Workforce Service, who enrolls the youth in Medicaid under the Chafee Option. |
| Wisconsin |
|
| X | A caseworker fills out the application, ideally with the youth. The documents are sent to the county economic support agency. A Medicaid packet is then sent to the youth’s address. The youth is not enrolled in Medicaid until he or she has selected a health plan by returning the packet. | |
| YOUTH ENROLLS ON HIS OR HER OWN | |||||
|
| Maryland |
|
| X | The youth goes to a family investment center to enroll; the caseworker will advise youth on what documentation to bring. |
| North Carolina |
|
| X | The youth is asked to go to the local county Division of Social Services to apply for Medicaid. It is assumed that Medicaid workers know about Medicaid under the Chafee Option—there are manual outlines specifying how to enroll the youth under the appropriate enrollment code. | |
continued
|
| State | Applicationa | Brief Descriptionb | ||
|---|---|---|---|---|---|
| None | Tailored | Standard | |||
| YOUTH ENROLLS ON HIS OR HER OWN (continued) | |||||
|
| Wyoming |
|
| X | Youth must fill out the standard Medicaid application and submit it to the Medicaid office. They may have the help of a Department of Children and Family caseworker or the caseworker may prod them to do it, typically within six months of leaving care. |
| a. Application refers to whether an application is required for Chafee enrollment and categorizes what type of application is used. A tailored application is one specifically for Chafee enrollment for youth aging out of foster care; typically it is significantly shorter and simpler than a normal Medicaid application. A standard application is used for Medicaid enrollment for all persons throughout the state. These applications typically ask about household members, other types of coverage, income and assets, etc. b. The brief descriptions include information from official documentation and conversations with knowledgeable staff. | |||||
APPENDIX E: Recertification Process by State
|
| State | Applicationa | Brief Descriptionb | |||
|---|---|---|---|---|---|---|
| None | Tailored | Medicaid | Multiple Benefits | |||
| YOUTH IS NOT INVOLVED OR HAS MINIMAL INVOLVEMENT IN THE RECERTIFICATION PROCESS | ||||||
| Complete Automation | Colorado | X |
|
|
| There is no renewal process; coverage continues without review up until age 21. |
| Louisiana | X |
|
|
| There is no renewal process; coverage continues without review up until age 21. | |
| Massachusetts | X |
|
|
| There is no renewal process; coverage continues without review up until age 21. | |
| Michigan | X |
|
|
| There is no renewal process; coverage continues without review up until age 21. | |
| Mississippi | X |
|
|
| There is no renewal process; coverage continues without review up until age 21. | |
| Missouri | X |
|
|
| There is no renewal process; coverage continues without review up until age 21. | |
| New Jersey | X |
|
|
| There is no renewal process; coverage continues without review up until age 21. | |
| South Carolina | X |
|
|
| There is no renewal process; coverage continues without review up until age 21. | |
| Washington | X |
|
|
| There is no renewal process; coverage continues without review up until age 21. | |
| Passive Renewal | Florida | X |
|
|
| There is no formal annual review process but the Medicaid eligibility worker checks the SACWIS annually to verify that the youth is still in the state and is not deceased. |
| Kansas |
| X |
|
| There is an annual renewal that the worker must complete (not the youth) to ensure the youth is under 21, not in jail, and still in the state. Youth are asked to maintain contact with their independent living worker; in the case of noncontact, the case is kept open absent of proof of ineligibility. | |
| North Carolina | X |
|
|
| The Medicaid caseworker must complete a redetermination every 12 months to determine continuation for Medicaid services under the Chafee Option. The redetermination is without regard to assets or income of the child through the month they turn age 21. | |
| Oregon |
| X |
|
| Youth are sent a packet annually to confirm address, but they are not required to return the packet. | |
| South Dakota | X |
|
|
| The youth is mailed a letter asking for address verification; if the letter is not returned with an updated address, it is presumed that the youth is still residing at that address and his/her Medicaid continues. | |
| Texas |
| X |
|
| Youth will receive a renewal packet in the mail that allows them to report any changes by mail, phone, or fax. However, they do not need to return the application. | |
| Ohio | X |
|
|
| A telephone interview is scheduled; the address is verified. If no contact is made, it is assumed that the youth is still eligible and Medicaid continues. | |
continued
|
| State | Applicationa | Brief Descriptionb | |||
|---|---|---|---|---|---|---|
| None | Tailored | Medicaid | Multiple Benefits | |||
| ANNUAL REVIEW WITH YOUTH INVOLVEMENT BUT NO REQUIRED DOCUMENTATION | ||||||
|
| Arizona |
|
|
| X | The Family Assistance Administration mails a letter to the youth asking for verification of information including residence and income (though there is no income eligibility for these youth). Youth may respond by phone to complete the recertification. The youth may also use the automated system to provide an updated address as needed. |
| California |
| X |
|
| There is an annual renewal; the youth will receive a half-page form asking if they want Medi-Cal to continue. If the youth does not return the form, the county is required to do a diligent search to find the youth prior to terminating Medicaid. Getting back on Medi-Cal takes an “easy” phone call. | |
| Connecticut |
|
|
| Xd | An annual renewal form is mailed to the youth; this is a standard Medicaid renewal form that asks for information including residence and income. If the youth is still receiving Department of Children and Family services, Medicaid is completed internally without the youth’s involvement. | |
| Georgia |
|
|
| Xd | A standard Medicaid form is mailed; youth may mail, fax, or call their case manager and complete the review over the phone. | |
| Rhode Island |
| X |
|
| Policy indicates that there is to be an annual notice mailed to youth for address verification. | |
| Wisconsin |
|
|
| X | An annual Medicaid/welfare renewal letter is mailed to the youth; this is mostly a residency check as there are no income requirements (but youth may need to fill out the income portion for other benefits). The youth may do the review online, by mail, by phone, or in person. | |
| Wyoming |
|
|
| X | Youth will receive a standard Medicaid renewal letter and must go in person to their local Department of Social Services office for renewal. They may seek help from their Independent Living coordinator. | |
| ANNUAL REVIEW WITH YOUTH INVOLVEMENT AND REQUIRED DOCUMENTATION | ||||||
|
| Indiana |
|
| Xc |
| Youth are mailed a letter asking them to provide proof of income, proof they are in school, and a birth certificate. The youth may return information by mail, may seek assistance at a local office, or may contact their case manager for help. |
| Iowa |
|
|
| Xd | Youth are mailed a standard Medicaid form that asks for income and residency. If the form is not returned, they are dropped from the program; there is no follow-up or direct contact between the Medicaid agency, the youth, or caseworker. | |
| Maryland |
|
|
| Xc | An annual review must be received with all necessary verification. All eligibility requirements must be met, including an income ceiling of 300% of the federal poverty level. | |
| Nevada |
|
|
| X | An annual renewal by mail includes a residency, income, and health insurance verification. The youth must mail the letter back to the Medicaid office. | |
continued
|
| State | Applicationa | Brief Descriptionb | |||
|---|---|---|---|---|---|---|
| None | Tailored | Medicaid | Multiple Benefits | |||
| ANNUAL REVIEW WITH YOUTH INVOLVEMENT AND REQUIRED DOCUMENTATION (continued) | ||||||
|
| New Mexico |
| X |
|
| Youth must fill out an annual renewal form and provide an ID, proof of citizenship/immigration, and social security number, and report if they have other health insurance. |
| Oklahoma |
|
| X |
| An annual renewal form is sent to the youth by mail to verify income and address; youth are requested to mail it back or go in person to the local Medicaid office. | |
| Utah |
|
| Xd |
| An annual renewal by mail checks whether the youth qualifies for another Medicaid category. The youth can do the renewal in person or online, or mail the letter back. | |
| a. Application refers to whether an application is required for Chafee recertification and categorizes what type of application is used. A tailored application is one specifically for Chafee recertification; typically it is significantly shorter and simpler than a normal Medicaid recertification and does not include income questions if the state has no income requirement for the Chafee Option. A Medicaid application is used for Medicaid recertification for all persons throughout the state. A multiple benefits application is used for recertification of multiple benefits, including but not limited to food stamps (SNAP). b. The brief descriptions include information from official documentation and conversations with knowledgeable staff about the process. c. We did not receive a copy of the form but this is our best guess from the interview. d. The state requires proof of income, expenses, or both be provided with the application. | ||||||
APPENDIX F: State Summaries of Medicaid Processes under the Chafee Option
(See end of table for definitions of columns and entries.)
| State | Year Implemented | Eligibility | Enrollment | Recertification | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Income/ Assets | Eligibility Hier-archy | Auto-matic | CW Assists | Youth Enrolls on Own | Forms Used | Auto-matic | Passive/ Internal | Active Renewal | Forms Used | ||
| a. Respondent’s best guess b. Pre-2005 but exact year unknown c. Began in 2005 but not fully implemented until 2007. d.Arizona removed its income restriction of 200% FPL in 2000 e. The state requires documentation additional to the form, as told by the respondent f. The state’s standard Medicaid redetermination forms must be submitted with proof of income attached. ELIGIBILITY: Income/assets refers to the income and asset limits some states require. FPL= federal poverty level. Eligibility Hierarchy indicates how states determine in which Medicaid coverage category to enroll youth who are eligible under multiple categories. First means that the youth is enrolled under the Chafee Option first, even if the youth is eligible under another category. SSI indicates that the youth will first be enrolled under SSI Medicaid, which is for those who are blind or disabled, if eligible; otherwise, they will be enrolled under the Chafee Option regardless of other eligibility. Last means the youth will be enrolled under the Chafee Option only if the youth is ineligible for Medicaid under every other category. ENROLLMENT: Automatic—automatic enrollment. CW Assists —a child welfare caseworker assists youth with enrollment. Youth Enrolls on Own —youth enrolls on his/her own. Forms Used—state uses an application form. Tailored—the application has been drawn up specifically for Chafee enrollment for youth aging out of foster care; typically it is significantly shorter and simpler than a normal Medicaid application. Standard—an application used for Medicaid enrollment for all persons throughout the state. RECERTIFICATION: Automatic —automatic recertification. Passive/Internal —recertification does not require much youth involvement. Active Renewal —youth is actively involved in the recertification process Forms Used —state uses an application form. Tailored—the application has been drawn up specifically for Chafee recertification; typically it is significantly shorter and simpler than a general Medicaid recertification and does not include income questions if the state has no income requirement for Chafee. Standard—refers to an application used for Medicaid recertification for all persons throughout the state. | |||||||||||
| Arizona | 2000 | --d | Last | X | Tailored | X | Standard | ||||
| California | 2000 | -- | SSI | X | -- | X | Tailored | ||||
| Colorado | 2007 | -- | SSI | X | -- | X | -- | ||||
| Connecticut | 2002a | -- | SSI | X | Tailored | X | Standardf | ||||
| Florida | 2006 | -- | SSI | X | -- | X | -- | ||||
| Georgia | 2008 | -- | SSI | X | -- | X | Standardf | ||||
| Indiana | 2006 | 200% FPL | SSI | X | n.a. | Xe | Standard | ||||
| Iowa | 2006 | 200% FPL | Last | X | -- | Xe | Standardf | ||||
| Kansas | 2004 | -- | Last | X | Tailored | X | Tailored | ||||
| Louisiana | 2008 | -- | SSI | X | -- | X | -- | ||||
| Maryland | 2009 | 300% FPL | Last | X | Standard | Xe | Standard | ||||
| Massachusetts | 2007a | -- | First | X | -- | X | -- | ||||
| Michigan | 2009 | -- | SSI | X | -- | X | -- | ||||
| Mississippi | 2005b | -- | SSI | X | -- | X | -- | ||||
| Missouri | 2007 | -- | Last | X | -- | X | -- | ||||
| Nevada | 2005 | -- | Last | X | Tailored | X | Standard | ||||
| New Jersey | 2001c | -- | Last | X | -- | X | -- | ||||
| New Mexico | 2006 | -- | SSI, Pregnant | X | Tailored | Xe | Tailored | ||||
| North Carolina | 2007 | -- | Last | X | Standard | X | -- | ||||
| Ohio | 2008 | -- | SSI | X | Tailored | X | Tailored | ||||
| Oklahoma | 2003 | 180% FPL | Last | X | Standard | Xe | Standard | ||||
| Oregon | 2010 | -- | First | X | Tailored | X | Tailored | ||||
| Rhode Island | 2007 | -- | SSI | X | -- | X | -- | ||||
| South Carolina | 2005 | -- | SSI | X | -- | X | -- | ||||
| South Dakota | 2003 | -- | First | X | -- | X | Tailored | ||||
| Texas | 2001 | 400% FPL, $10,000 | Last | X | -- | X | Tailored | ||||
| Utah | 2006 | -- | Last | X | Standard | X | Standardf | ||||
| Washington | 2007 | -- | SSI | X | -- | X | Standard | ||||
| Wisconsin | 2008 | -- | SSI | X | Standard | X | -- | ||||
| Wyoming | 2003 | -- | SSI | X | Standard | X | Standard | ||||
1. States included in the report had taken the Chafee Option as of January 2011.
2. PL 111-148, Section 10201.
3. In 2008 the Fostering Connections to Success and Increasing Adoptions Act gave states the option to extend foster care until ages 19, 20, or 21. To date 11 states have submitted state plan amendments with three—Alabama, Illinois and Maryland —approved to date.
4. Other states have expanded Medicaid coverage through other means, including waivers (see Patel and Roherty 2007, for detailed discussion).
5. In addition to youth in care on their 18th birthday, Florida extended coverage to “young adults who have been adopted from foster care after age 16 who have spent a minimum of six months in foster care within the twelve months immediately preceding adoption and young adults who have been placed with a court-approved dependency guardian, who have spent a minimum of six months in foster care within the twelve months immediately preceding the placement” (Lewis 2008).
6. We use the term SACWIS generically to represent a state’s child welfare information system.
7. Some counties in California do not have computerized administrative data systems, and independent living workers will therefore connect youth to the eligibility worker directly.
8. At this time, we have not received recertification forms from Indiana and Maryland.
9. Results from linear probability models are available from the authors upon request.
10. Data do not exist that track the percentage of youth staying in care past 18. We approximate this percentage using data from the Adoption and Foster Care Reporting System by taking the percentage of youth age 18 in care in a state in FY2007 divided by the number of youth in care in that state at age 17 in FY2006.
11. This includes a 5 percent disregard required of all states. Income will be based on a modified adjusted gross income as defined by federal income tax filings.
12. Youth formerly in foster care who lose a job that provided health insurance would still be eligible for Medicaid until age 26; however, flags in the Medicaid system will not alert the agency to the youth’s eligibility until the youth applies for Medicaid.
13. For a detailed discussion of the implications and consequences of a fee-for-service versus a managed care system, see Howell, Palmer, and Adams (2012).
14. A few states that had appeared in some sources as taking the option had in fact not taken it.
15. To be eligible for the Chafee Option, youth must have been in care on their 18th birthday. Due to concerns about how eligibility might be recorded in the month in which a youth turns 18, we chose to identify foster youth at age 17 years, 11 months, under the assumption that few youth in care at that point leave care before their 18th birthday.
16. At the time this analysis was conducted, data were available through FY2008.
17. Examination of the linked files indicated potential problems around the turn of the fiscal year. To reduce the potential for miscoding continuity of enrollment for youth turning 18 around the changing fiscal year, we did not include youth with birthdays in August or September (i.e., the sample includes only youth with 18th birthdays in October 2005 through July 2006).
