ABSTRACT: Residential treatment facilities are a key component of states' behavioral health systems. They form part of the spectrum of treatment for both mental and substance use disorders (M/SUDs). Residential treatment includes providing health services or treatment in a 24-hour-a-day, 7-day-a-week structured living environment for individuals who need support for their mental health or substance use recovery before living on their own, but where inpatient treatment is not needed. Care is provided for limited periods of time and has the goal of preparing people to move into the community at lower levels of care.
Residential M/SUD treatment settings are governed almost exclusively by state statutes and regulations, rather than by federal laws. The Compendium describes regulatory provisions and Medicaid policy for residential treatment in all 50 states and the District of Columbia (hereafter states) and contains links to detailed summaries of state licensure and oversight standards and, separately, state Medicaid requirements. The supporting research examined residential treatment from a legal perspective, focusing foremost on state statutes and regulations, supplemented by other documents and input from states.
This report was prepared under contract #HHSP2332016000231 between HHS's ASPE/BHDAP and IBM Watson Health. For additional information about this subject, you can visit the BHDAP home page at https://aspe.hhs.gov/bhdap or contact the ASPE Project Officers at HHS/ASPE/BHDAP, Room 424E, H.H. Humphrey Building, 200 Independence Avenue, S.W., Washington, D.C. 20201; Joel.Dubenitz@hhs.gov, Judith.Dey@hhs.gov.
DISCLAIMER: The opinions and views expressed in this report are those of the authors. They do not reflect the views of the Department of Health and Human Services, the contractor or any other funding organization. This report was completed and submitted on June 10, 2020.
TABLE OF CONTENTS
SECTION 1. INTRODUCTION
- Methodology
- Organization of the Report
SECTION 2. OVERVIEW OF THE NONMEDICAID RESIDENTIAL TREATMENT REGULATIONS
- Domains Regarding Processes of Oversight
- Domains Regarding Facility Operations
SECTION 3. OVERVIEW OF STATE MEDICAID REQUIREMENTS FOR RESIDENTIAL TREATMENT
- Sources of State Medicaid Authority to Reimburse Residential Treatment
- Domains Regarding Processes of Oversight
- Domains Regarding Facility Operations
SECTION 4. DISCUSSION AND SYNTHESIS
- Oversight
- Operations
- Other Key Findings
APPENDICES
- APPENDIX A: Detailed Tables
- APPENDIX B: Separate State Summaries
- APPENDIX C: Detailed Methodology
LIST OF FIGURES
- FIGURE 1: Domains and Subdomains of Oversight and Operation of Residential Treatment Facilities
- FIGURE 2: Categories of Regulated Residential Treatment Facilities
- FIGURE 3: Number of States with Some Level of Identified Oversight of Residential Treatment Facilities
- FIGURE 4: Number of States with Inspections of Residential Treatment Facilities
- FIGURE 5: Number of States with Provisions for Placement Criteria Specific to Residential Treatment
- FIGURE 6: Number of States with Provisions for Treatment and Discharge Planning Specific to Residential Treatment
- FIGURE 7: Number of States with Provisions for Aftercare Specific to Residential Treatment
- FIGURE 8: Number of States with Requirements for Evidence-Based Treatments Specific to Residential Treatment
- FIGURE 9: Number of States with Provisions for MAT Specific to Residential Treatment
- FIGURE 10: Number of States with Provisions for Staffing Levels Specific to Residential Treatment
- FIGURE 11: Number of States with Provisions for QA/QI Specific to Residential Treatment
- FIGURE 12: Number of States with Provisions for Treatment of Co-occurring Disorders Specific to Residential Treatment
LIST OF TABLES
- TABLE 1: Number of States Regulated and Licensed by Funding Source
- TABLE 2: Number of States Using Different Approaches to Licensure and Other Oversight
- TABLE 3: Number of States with Requirements for Ongoing or Cause-Based Inspections
- TABLE 4: Number of States with Regulatory Provisions Regarding Wait Times
- TABLE 5: Number of States by Staffing Standards for Licensure
- TABLE 6: Numbers of States by Training Requirements for Licensure
- TABLE 7: Residential Treatment Facilities Using Workforce Quality Assurance Practices as Standard Operating Procedure, Mental Health 2010, SUD 2013
- TABLE 8: Number of States Regulating Placement Criteria
- TABLE 9: Number of States with Requirements Regarding Treatment or Discharge Planning or Aftercare Services
- TABLE 10: Number of States with Regulations Regarding Services
- TABLE 11: Number of States with Regulations Regarding MAT Specific to Residential Treatment
- TABLE 12: Number of States with Regulations Regarding Service Recipient Rights
- TABLE 13: Number of States with QA/QI Regulations
- TABLE 14: Number of States with Governing Body Regulations
- TABLE 15: Number of States with Regulations Regarding Special Populations
- TABLE 16: Sources of State Medicaid Authority to Reimburse Behavioral Health Treatment in IMDs, Number of States
- TABLE 17: Number of States With Different Categories of Residential Mental Disorder Treatment Facilities That Can Enroll in Medicaid
- TABLE 18: Number of States with Different Categories of Residential SUD Treatment Facilities That Can Enroll in Medicaid
- TABLE 19: Number of States with Different Processes of Medicaid Enrollment Fully or Partially Present
- TABLE 20: Number of States with Medicaid Requirements for Staffing in Residential Facilities
- TABLE 21: Number of States with Medicaid Requirements for Staff Training in Residential Facilities
- TABLE 22: Number of States with Medicaid Requirements for Placement in Residential Facilities
- TABLE 23: Number of States with Medicaid Requirements for Treatment and Discharge Planning, Care Coordination, and Aftercare in Residential Treatment
- TABLE 24: Number of States with Medicaid Requirements for Services in Residential Facilities
- TABLE 25: Number of States with Medicaid Requirements for MAT in Residential Facilities
- TABLE 26: Number of States with Medicaid Requirements for QA/QI
- TABLE 27: Number of States with Medicaid Requirements Related to Special Populations
- TABLE A1: Categories of Regulated Residential Mental Health Treatment Facilities
- TABLE A2: Categories of Regulated Residential SUD Treatment Facilities
- TABLE A3: Regulation of Residential Mental Health Treatment Facilities Based on Funding
- TABLE A4: Regulation of Residential SUD Treatment Facilities Based on Funding
- TABLE A5: Extent of Regulation of Residential Mental Health and SUD Treatment Facilities by State
- TABLE A6: Organization of Oversight Within States
- TABLE A7: Processes of Licensure and Basic Oversight for Mental Health
- TABLE A8: Processes of Licensure and Basic Oversight for Substance Use
- TABLE A9: Ongoing or Cause-Based Monitoring
- TABLE A10: Wait Time Standards for Residential Facilities
- TABLE A11: Staffing Standards for Residential Facilities for Mental Health
- TABLE A12: Staffing Standards for Residential Facilities for Substance Use
- TABLE A13: Staff Training Standards for Residential Facilities
- TABLE A14: Placement Standards for Residential Facilities for Mental Health
- TABLE A15: Placement Standards for Residential Facilities for Substance Use
- TABLE A16: Treatment Planning, Discharge Planning, and Aftercare Standards for Residential Facilities for Mental Health
- TABLE A17: Treatment Planning, Discharge Planning, and Aftercare Standards for Residential Facilities for Substance Use
- TABLE A18: Treatment Services Standards for Residential Facilities
- TABLE A19: Requirements Specific to MAT in Residential Facilities
- TABLE A20: Service Recipient Rights--Grievances and Complaints Standards for Residential Facilities
- TABLE A21: Service Recipient Rights--Restraint and Seclusion Standards for Residential Facilities
- TABLE A22: QA/QI Standards for Residential Facilities
- TABLE A23: Governance Standards for Residential Facilities
- TABLE A24: Requirements Specific to Special Populations for Residential Facilities
- TABLE A25: Source of State Medicaid Authority to Reimburse Residential Mental Health Treatment in IMDs
- TABLE A26: Source of State Medicaid Authority to Reimburse Residential SUD Treatment in IMDs
- TABLE A27: Categories of Residential Mental Health Treatment Facilities That Can Enroll in Medicaid
- TABLE A28: Categories of Residential SUD Treatment Facilities That Can Enroll in Medicaid
- TABLE A29: Processes of Medicaid Enrollment
- TABLE A30: Medicaid Staffing Standards for Residential Facilities
- TABLE A31: Medicaid Staff Training Standards for Residential Facilities
- TABLE A32: Medicaid Placement Standards for Residential Facilities
- TABLE A33: Medicaid Treatment Planning, Discharge Planning, Care Coordination, and Aftercare Standards for Residential Facilities
- TABLE A34: Medicaid Treatment Services Standards for Residential Facilities
- TABLE A35: Medicaid Requirements Specific to MAT in Residential Facilities
- TABLE A36: Medicaid QA/QI Standards for Residential Facilities
- TABLE A37: Medicaid Requirements Specific to Special Populations for Residential Facilities
ACKNOWLEDGMENTS
IBM Watson Health prepared this report under contract to the Office of the Assistant Secretary for Planning and Evaluation (ASPE), U.S. Department of Health and Human Services (HHS) (HHSP2332016000231HHSP23337003T). The authors appreciate the guidance of Judy Dey and Joel Dubenitz (ASPE). Jesse Roberts (IBM Watson Health), Wendolyn Ebbert (Brandeis University), and Danielle Strauss (Brandeis University) contributed to important phases of data collection. Mary Beth Schaefer, Paige Jackson, and Kristin Schrader (IBM Watson Health) provided editorial support. Special thanks are owed to Ted Lutterman and Kristin Neylon at NRI and to Melanie Whitter and Marcia Trick at National Association of State Alcohol and Drug Abuse Directors (NASADAD), both for their subject matter expertise and their invaluable assistance in contacts with states for validation of the primary summaries. We also thank our key informants: Lindsey Browning, the National Association of Medicaid Directors; Pamela Greenberg, the National Association of Behavioral Health and Wellness; Dr. Joe Parks, the National Council for Behavioral Health; Ted Lutterman, NRI; and Melanie Whitter and Rick Harwood, NASADAD.
The views and opinions expressed here are those of the authors and do not necessarily reflect the views, opinions, or policies of ASPE or HHS. The authors are solely responsible for any errors.
ACRONYMS
The following acronyms are mentioned in this report and/or Appendix A and Appendix C. Appendix B has an extensive acronym list that is not included here.
| ASAM | Americans Society of Addiction Medicine |
|---|---|
| ASO | Administrative Service Organization |
| ASPE | HHS Office of the Assistant Secretary for Planning and Evaluation |
| AUD | Alcohol Use Disorder |
| CHIP | Children's Health Insurance Program |
| CMS | HHS Centers for Medicare & Medicaid Services |
| COA | Council on Accreditation |
| CON | Certificate of Need |
| DSH | Disproportionate Share Hospital |
| HHS | U.S. Department of Health and Human Services |
| IDU | Injection Drug Use |
| IMD | Institution for Mental Disease |
| IRTS | Intensive Residential Treatment Services |
| LOCUS | Level of Care Utilization System |
| M/SUD | Mental and Substance Use Disorders |
| MACPAC | Medicaid and CHIP Payment and Access Commission |
| MAT | Medication-Assisted Treatment |
| MCE | Managed Care Entity |
| N-MHSS | National Mental Health Services Survey |
| N-SSATS | National Survey of Substance Abuse Treatment Services |
| NASADAD | National Association of State Alcohol and Drug Abuse Directors |
| OUD | Opioid Use Disorder |
| QA/QI | Quality Assurance/Quality Improvement |
| PPW | Pregnant and Parenting Women |
| R/S | Restraint/Seclusion |
| SAMHSA | HHS Substance Abuse and Mental Health Services Administration |
| SMI | Serious Mental Illness |
| SUD | Substance Use Disorder |
| SUPPORT | Substance Use Disorder Prevention that Promotes Opioid Recovery and Treatment for patients and communities act |
| TJC | The Joint Commission |
| WM | Withdrawal Management |
EXECUTIVE SUMMARY
Background
Residential treatment facilities are a key component of states' behavioral health systems. They form part of the spectrum of treatment for both mental and substance use disorders (M/SUDs). Residential treatment involves providing health services or treatment in a 24-hour-a-day, 7-day-a-week structured living environment for individuals who need support for their mental health or substance use recovery before living on their own, but where inpatient treatment is not needed. Care is provided for limited periods of time and has the goal of preparing people to move into the community at lower levels of care.[1]
Recently, more attention has been paid to these intermediate levels of care for persons with M/SUD. The Centers for Medicare & Medicaid Services (CMS) has expanded efforts to ensure a broader continuum of care for both M/SUD, including demonstration opportunities for state Medicaid programs to receive federal matching funds for an expanded range of services that include residential treatment. On July 27, 2015, and November 1, 2017, CMS announced opportunities for states to design new substance use disorder (SUD) service delivery systems using the Section 1115 demonstration authority under Medicaid.[2, 3] Among other things, these opportunities enabled approved states to expand reimbursement for residential SUD treatment. More recently, on November 13, 2018, CMS announced similar opportunities regarding service delivery systems for adults with a serious mental illness (SMI). Improving quality is a key component of those demonstrations.[4]
Residential M/SUD treatment settings are governed almost exclusively by state statutes and regulations, rather than by federal laws. This Compendium's purpose is to inform behavioral health treatment policy by providing detailed information about each state's approach to regulating and funding services in residential M/SUD treatment settings. The Compendium describes regulatory provisions and Medicaid policy for residential treatment in all 50 states and the District of Columbia (hereafter states) and contains links to detailed summaries of state licensure[5] and oversight standards and, separately, state Medicaid requirements. The supporting research examined residential treatment from a legal perspective, focusing foremost on state statutes and regulations, supplemented by other documents and input from states.
In reading this Compendium, however, it is critical to remember that states may use other levers of oversight in addition to regulations, such as contracts with facilities receiving state funds, contracts between the state and Medicaid managed care entities (MCEs) or individual providers, and contracts between MCEs and individual providers. State licensure manuals and state Medicaid policies also are used to define provider responsibilities. Additionally, all state Medicaid programs require appropriate licensure of providers, hence, incorporating by that mandate all relevant requirements for obtaining and maintaining licensure.
Methodology
As a precursor to the collection and synthesis of data drawn primarily from state law, we conducted an environmental scan[4] and interviewed experts in the field. We then examined relevant statutes and regulations governing behavioral health treatment and licensing or certification for the 51 states, as well as examining state Medicaid requirements regarding residential treatment. The domains examined for both licensure and Medicaid relate to standards: (1) regarding processes of oversight such as regulation and licensure; and (2) related to facility operation that are conditions of operation and licensure.
The primary focus of this Compendium is residential M/SUD treatment for adults ages 21-64 years. For this Compendium, we define residential treatment as clinical treatment services for M/SUD provided in a 24-hour living environment, including withdrawal management residential facilities. This Compendium excludes residential settings that predominantly serve people with intellectual and other developmental disabilities or settings that are forensic, correctional, or inpatient.
Research Findings
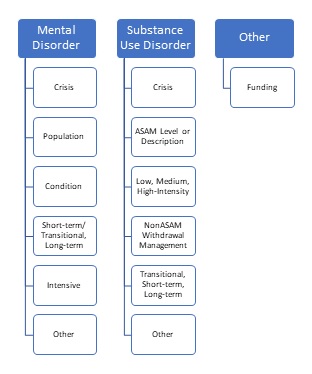
Processes of oversight. From state to state, regulations and Medicaid policy vary dramatically in how states define residential treatment settings. The largest category of mental health residential facilities among states comprises those that are crisis focused. In the realm of SUD residential treatment, the categories identified in the American Society of Addiction Medicine (ASAM) criteria as Level 3 residential and withdrawal management facilities form a substantial portion of state facility types. Other states focus on, for example, the duration of stay or the condition treated. Regulatory processes sometimes vary between states by funding type (e.g., publicly-funded, Medicaid-enrolled, private facilities). In addition, many states have multiple agencies or subagencies overseeing and/or licensing treatment facilities, including separate entities regulating mental disorder versus SUD treatment, separate entities overseeing Medicaid-enrolled facilities, and layers of regulation that may include a state behavioral health agency, a state public health department, and a state Medicaid agency. Mental health residential treatment is less likely than SUD residential treatment to be regulated, although determining which facilities in the states are unregulated is difficult. Doing so requires a thorough understanding of which types of facilities are regulated. From that, one can conclude that certain facility types are or may be unregulated, if they exist in the state.
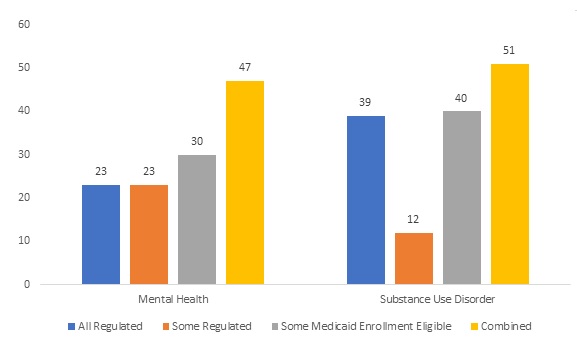
The licensure process can be quite complex and entail many requirements. Accreditation by an independent body is somewhat unlikely to be required; it is more likely that a state will confer "deemed status" on facilities that are accredited, absolving them of certain licensure requirements. Often the requirement being excused relates to some portion of licensure inspections, most often at renewal. Viewing inspections as an indicator of the state's ability to monitor facilities over time, whether as part of licensure, renewal, or for cause, we closely examined the extent to which states have some provision for inspection, whether through licensure and related standards or as part of Medicaid enrollment. We found such requirements for 47 and 50 states, for mental disorder and SUD treatment, respectively.
Standards for facility operations. This study examined many aspects of facility operation that may be addressed via regulation. We found that some, such as wait time requirements for placement, are often not included in regulations but may be found in contracts or on agency websites. Other operational considerations are frequently addressed in a regulatory context. Some primary findings are summarized below.
Placement in the appropriate setting and level of care is important to ensure that patients receive the care they need. We examined whether there were specific state criteria for placement and/or assessment, to ascertain whether placement in a given residential facility type is suitable for the individual seeking treatment. Specific placement criteria for residential treatment facilities are the norm, derived from a combination of licensure-related and Medicaid requirements; 42 and 50 states were found to include such requirements for mental disorder and SUD residential treatment, respectively. As might be expected, required use of the ASAM Patient Placement Criteria was nearly exclusively limited to residential SUD treatment. A total of 45 states specifically use the ASAM criteria for placement in SUD treatment; many of those 45 states have Section 1115 Institution for Mental Diseases (IMD) demonstrations. Many states also have, in addition to standards of placement, criteria for continued stay and/or discharge.
States are more likely to include treatment planning and discharge planning requirements in licensure and related standards than they are to include them as Medicaid requirements. Documentation examined revealed that treatment planning requirements were included for 46 and 50 states, respectively, for mental disorder and SUD residential treatment. Nearly as many states included discharge planning requirements: 40 and 49 states for mental disorder and SUD treatment, respectively. These high numbers indicate the importance placed on appropriately planning treatment and the provision for ongoing treatment and support after discharge, preferably beginning early in the treatment process.
Even though discharge planning requirements are common, state standards for the actual provision of aftercare services by a residential facility as a bridge to subsequent care or follow-up after discharge from a residential facility are rare. Six and 13 states include such requirements for mental disorder and SUD residential treatment, respectively, primarily in licensure or other nonMedicaid standards and most frequently requiring follow-up rather than aftercare.
Ensuring the provision of evidence-based or best practice treatment is crucial to maintaining high-quality residential services for M/SUDs. In addition to assessments related to placement, treatment planning, and coordination of care, treatment services in the form of psychosocial and medication treatment are key components of residential treatment. Although states vary in the extent to which they elaborate, in the SUD treatment realm, the ASAM Level 3 standards increasingly are adopted to guide state treatment requirements, driven in part by approved Section 1115 Medicaid demonstrations. These standards set criteria for different levels of residential and withdrawal management treatment. Two discrete indicators of service requirements that were examined as part of this study were requirements for use of: (1) evidence-based practices generally; and (2) medication-assisted treatment[6] (MAT) specifically, in residential treatment. Regarding the first, we found that SUD residential treatment facilities are most likely to have requirements for evidence-based practices, with 43 out of 51 states including some form of requirement, most commonly MAT. In contrast, only 16 states, in total, incorporated requirements specific to evidence-based practices for residential mental health treatment. Regarding MAT, requirements were more commonly specific to SUD treatment facilities, with a total of 39 states having SUD licensure-related and/or Medicaid-related requirements in place in regulations or other documents specific to residential treatment. A significant portion of the Medicaid requirements reflect the existence of Section 1115 demonstrations.
Staffing standards may include requirements regarding hiring, credentialing, training, documentation of employment requirements or practices, and staffing levels, among other things. As one indicator of state involvement in staffing standard-setting, we looked at staffing levels. Adequate staffing levels are needed to ensure quality treatment and safety in 24-hour mental disorder and SUD treatment settings. Among requirements for mental health residential treatment, 30 states had general requirements for "adequate" or "sufficient" staffing and 27 had specific ratio requirements. For SUD residential treatment, 41 states had general requirements and 34 had specific ratio requirements. Most such requirements sprang from licensure and other nonMedicaid standards.
The scope and nature of quality assurance/quality improvement requirements applicable to residential M/SUD treatment vary considerably, but some form of explicit requirement imposed on facilities is common (e.g., written quality improvement plan, use of data for quality improvement purposes). This is truer for SUD than for mental disorder treatment and generally originates in licensure and related oversight standards rather than in state Medicaid requirements. We identified 38 and 48 states that impose some such requirement for residential mental disorder and SUD treatment facilities, respectively.
We looked at two discrete aspects of service recipient rights, related to: (1) the right to voice grievances, taken as an indicator of the ability of service recipients to enforce their rights in general; and (2) rights related to restraint and seclusion, because restraint and seclusion affect safety and dignity. The first--the right to voice grievances--is most commonly mandated, with 37 and 42 states having such requirements for mental disorder or SUD treatment, respectively, as part of licensure standards. In contrast, rights regarding restraint or seclusion were found for mental disorder or SUD treatment in 42 and 37 states, respectively.
Governance standards are elaborate in some states and nonexistent in others. They may be integrated into licensure requirements, for example, as part of what facilities must demonstrate in their application. They also may be a more general part of state regulations governing operating requirements. They may be as simple as requiring information at licensure and the development and maintenance of policies and procedures, or they may include detailed requirements regarding different areas of facility internal structure and oversight. Some form of governance requirements were located in licensure standards in 36 states regarding mental disorder residential treatment and in 41 states regarding SUD residential treatment.
States identify a range of special populations to whom they wish to target services. This is truer of SUD treatment than of mental disorder treatment and often stems from block grant requirements. The two most common populations identified, particularly for SUD residential treatment, are those with co-occurring M/SUDs and pregnant and parenting women or parents of dependent children. Regarding the latter, many states have specific requirements for residential facilities in which pregnant women, parenting women, and/or families with dependent children may receive treatment, including educational, health, and safety requirements for children. Regarding standards applicable to treating those with co-occurring M/SUDs, although additional requirements may exist in contracts or policy documents, in the documentation reviewed, we found nearly twice as many states with licensure-related requirements for treatment of co-occurring M/SUD disorders stemming from the SUD side of state policy (29 states) compared with mental disorder residential treatment (15 states). Many of the former reflect requirements based in Section 1115 demonstrations but states have, apart from that, often sought to ensure that SUD-focused treatment facilities address mental disorders as well.
Other key findings. This research also produced at least four overarching additional findings.
-
State Medicaid programs all incorporate some requirement for appropriate licensure within the state, for facilities providing residential treatment. This allows state Medicaid regulations to be less exacting in many cases, because they rely on already existing standards.
-
Section 1115 demonstrations, as well as the ASAM criteria, have been critical to strengthening regulation of residential SUD treatment. The state structure and oversight of residential mental disorder treatment has not kept pace.
-
We did not include all residential settings in this study. For example, small group homes and recovery housing, where clinical treatment is not integrated into the residence, were excluded. Such facilities may or may not be regulated or licensed. They may be providing very valuable benefits to their residents or services of unknown quality.
-
States have diverse ways of overseeing M/SUD treatment. Some rely heavily on published statutes and regulations. This results in clearly established, transparent requirements that lay out the legal basis for oversight, licensure, and/or Medicaid enrollment. It also may result in requirements being established that can be difficult to change when flexibility or adaptation is needed. Comparable to promulgated regulations are state Medicaid demonstration or state plan documents that have been approved by CMS, which are binding and have the benefit of transparency and certainty, provided rapid change is not required. Some states rely more heavily on contractual requirements, also binding but often less transparent. States also use agency licensing or standards manuals and, for Medicaid, provider manuals or other policy documents. Theoretically, these may be less binding on providers unless, as is often the case, they are incorporated by reference into state statutes, regulations, or provider agreements. This approach has the benefit of requiring only that the manual or other document be amended and published to alter requirements when doing so may be time sensitive. However, hurdles can exist that impede public access to such documents.
Conclusions
Regulation and oversight of residential treatment is a patchwork, and identification of unregulated facilities is an imprecise exercise. Regulation of SUD treatment is more pronounced and somewhat more consistent across states than is regulation of mental disorder treatment, although both have room for improvement. This difference is often driven by the fact that many of the SUD treatment requirements are a result of Medicaid demonstration/waiver requirements that also appear to be seeping into SUD licensure and other nonMedicaid oversight standards. The inclusion of requirements as part of Medicaid demonstrations, such as requirements regarding provision of MAT in residential treatment, even if only directly applicable to certain facilities or certain populations, means that it is more likely that other facilities and individuals in the state will experience spillover as MAT becomes more widely available. This suggests that, if more states obtain approval for Section 1115 demonstrations that affect reimbursement of mental disorder treatment in IMDs in accordance with the November 2018 State Medicaid Directors Letter,[4] it is possible that similar strides could take place for mental disorder residential treatment. Additionally, the Section 1115 demonstrations are laboratories for innovation that may spread best practices to other states. Consideration of how to create more such laboratories for the treatment of SMI is an important next step.
SECTION 1. INTRODUCTION
Residential treatment facilities are a key component of states' behavioral health systems. They form part of the spectrum of treatment for both mental and substance use disorders (M/SUDs). Residential treatment involves providing health services or treatment in a 24-hour, 7-day a week structured living environment for individuals who need support for their mental health or substance use recovery before living on their own, but where inpatient treatment is not needed. Care is provided for limited periods of time and has the goal of preparing people to move into the community and into lower levels of care.[1]
The Substance Abuse and Mental Health Services Administration's (SAMHSA's) National Mental Health Services Survey (N-MHSS) for 2017 reported that the United States had 856 organizations providing residential mental health treatment for adults. Eighty percent of adult residential treatment facilities offered psychotropic medications, 65% offered group psychotherapy, 60% offered individual psychotherapy, and 58% offered cognitive behavioral therapy.[7] More than 80% of these facilities provided only mental health services, whereas 19% also provided substance use services. Most facilities were nonprofit and accepted Medicaid payments.[8]
The SAMHSA National Survey of Substance Abuse Treatment Services (N-SSATS) survey for 2017 found that approximately 3,125 organizations were providing residential substance use disorder (SUD) treatment in the United States.[9] Among all residential substance use facilities, about 23% of these facilities had fewer than 13 residential beds, 59% of facilities had more than 18 residential beds, and 18% had 48 or more residential beds.[10] Most residential SUD treatment facilities were nonprofit. About half accepted Medicaid and more than 60% accepted private insurance.[9]
Recently, increased attention has been paid to these intermediate levels of care for persons with M/SUD. The Centers for Medicare & Medicaid Services (CMS) has expanded efforts to ensure a broader continuum of care for both M/SUD, including demonstration opportunities for state Medicaid programs to receive federal matching funds for an expanded range of services that include residential treatment. On July 27, 2015, and November 1, 2017, CMS announced opportunities for states to design new SUD service delivery systems using the Section 1115 demonstration authority under Medicaid.[2, 3] Among other things, these enabled approved states to expand reimbursement for residential SUD treatment. More recently, on November 13, 2018, CMS announced similar opportunities regarding service delivery systems for adults with a serious mental illness (SMI).
Improving access to needed treatment and quality care are key components of the Section 1115 demonstrations.[4] For SUD treatment generally, this has been shaped by the demonstration requirements that treatment follow aspects of the American Society of Addiction Medicine (ASAM) treatment criteria, and the ASAM criteria have increasingly made their way into state Medicaid and nonMedicaid requirements as a result. The ASAM criteria were developed to improve assessment, treatment and recovery services, and to match patients to the appropriate level of treatment. For adult residential treatment, this includes the following levels:
- Level 3.1. Clinically Managed Low-Intensity Residential Services.
- Level 3.3. Clinically Managed Population-Specific High-Intensity Residential Services (formerly Medium-Intensity).
- Level 3.5. Clinically Managed High-Intensity Residential Services.
- Level 3.7. Medically Monitored High-Intensity Inpatient Services (which, in many states, are offered in residential settings).
- Level 3.2-WM. Clinically Managed Residential Withdrawal Management.
- Level 3.7-WM. Medically Monitored Inpatient Withdrawal Management (in many states, offered in residential settings).
A similar system of levels of care and placement criteria exists for mental health treatment in the Level of Care Utilization System (LOCUS):
- Level 5. Medically Monitored Residential Services.
- Level 6. Medically Managed Residential Services.[11]
According to expert interviews, states are increasingly requiring the LOCUS for placement purposes in their contracts with providers or managed care entities (MCEs).
Control and oversight of residential behavioral health treatment settings, including with regard to placement, quality, treatment services, and other matters, however, are fundamentally governed by state laws and regulations, and these vary by state. Indeed, some states may have multiple sets of oversight, licensure, or certification requirements, and some licensure standards also may require accreditation or provide for optional accreditation. Thus, accreditation by an independent accrediting body such as the Joint Commission (TJC), the Commission on Accreditation for Rehabilitative Facilities, or the Council on Accreditation (COA) can provide yet another layer of oversight and inspection, beyond that carried out by the states. This Compendium describes regulatory provisions and Medicaid policy for residential treatment in all 50 states and the District of Columbia (hereafter states). Appendix B contains links to detailed summaries of state licensure and oversight requirements and state Medicaid requirements, including Section 1115 demonstration requirements.
The primary focus of this Compendium is residential M/SUD treatment for adults ages 21-64 years. As more fully explained under Methodology, this Compendium does not include residential settings that predominantly serve people with intellectual and other developmental disabilities or settings that are forensic or correctional. It also does not include residential placements that are not required to include some form of clinical psychosocial treatment for mental disorders or SUDs, although withdrawal management facilities are included. States use many terms for residential treatment settings. This Compendium uses the term residential treatment as a generic label that encompasses all state licensure categories; the state summaries use each state's specific licensure or certification term(s).
The Compendium's purpose is to inform residential behavioral health treatment policy by providing detailed information about each state's approach to regulating and funding services in residential behavioral health treatment settings. In reading this Compendium, however, it is critical to remember that states may use other levers of oversight in addition to regulations, such as contracts with facilities receiving state funds, contracts between the state and Medicaid MCEs or individual providers, or contracts between MCEs and individual providers. State licensure manuals and state Medicaid policies also are used to define provider responsibilities. Additionally, all state Medicaid programs require appropriate licensure of providers, incorporating by that mandate all relevant requirements for obtaining and maintaining licensure.
Methodology
As a precursor to the collection and synthesis of data drawn primarily from state law, we conducted an environmental scan and interviewed experts in the field. Relevant articles and other source documents were reviewed, synthesized, and summarized in the environmental scan, which is published separately.[12] In addition, we identified and interviewed a number of subject matter experts who are recognized in the acknowledgments section of this Compendium.
On the basis of findings from the environmental scan[12] and interviews with experts, we developed a template that provided the coding structure for data collected throughout the project. Relevant statutes and regulations governing behavioral health treatment and licensing or certification from 51 jurisdictions were reviewed and abstracted into the data collection template. We prepared detailed state summaries of: (1) licensure standards; and (2) Medicaid requirements by synthesizing the abstracted information (see Appendix B).
Several parameters were placed around the scope of data collection to ensure consistency:
- Residential treatment was defined as clinical treatment services provided in a 24-hour living environment, including withdrawal management treatment.
- Only residential treatment facilities for adults were included; thus, treatment specific to children or adolescents was excluded.
- We excluded facilities that are associated with the criminal justice system or that are in inpatient settings.
- Medicaid-specific requirements are included separately for each state.
The state summaries that resulted from data collection regarding licensure were shared with the individual states for validation. On the basis of input from the states, the summaries were revised as necessary. In some instances, state personnel provided additional sources of information beyond the statutes and regulations and, to the extent that it was pertinent to the study, we included that information. Among other things, this included information in certification or licensure manuals and written input from state staff. All publicly available documents on which we relied are referenced in the state summaries.
In the summaries of state Medicaid requirements, we primarily relied on state Medicaid regulations and Section 1115 demonstration documents. Where necessary, these were supplemented with additional sources. The relative absence of certain requirements in state Medicaid regulations, however, does not mean that Medicaid programs do not have service requirements in provider agreements with Medicaid or MCEs, provider manuals, or elsewhere. Similarly, some states may passively rely on the presence of licensure requirements to ensure that service standards are in place.
Throughout the study, we used a legal mapping framework. This approach provides structured steps to follow in reviewing and compiling information from legal documents. In addition, we coordinated with other federal efforts on this topic and leveraged efficiencies available through ongoing parallel efforts, such as those being led by the Medicaid and CHIP Payment and Access Commission (MACPAC).[13] By integrating input from leaders in this field throughout the course of the project, as well as applying a rigorous legal mapping framework for abstraction and synthesis, we generated accurate information to disseminate widely and inform next steps in addressing capacity for M/SUD treatment across the continuum of care (see Appendix C for more detailed description of the methods for this Compendium).
Conceptual framework. This study examines residential treatment from a legal perspective, focusing foremost on state statutes and regulations. The domains examined relate to regulatory standards: (1) regarding processes of oversight such as regulation and licensure;[14] and (2) related to facility operation that are conditions of operation and licensure. Figure 1 identifies those domains and subdomains, all of which are described and discussed more fully in Section 2 of this Compendium. Complementing this, Section 3 uses some but not all of the same domains and subdomains in the context of state Medicaid requirements.
Study limitations. One limitation is that a full understanding of a state's oversight of residential treatment facilities requires examination of more than the state statutes and regulations, which provide only a partial picture of how oversight works in reality. Those statutes and regulations are, however, the legally enforceable mechanisms that govern facilities, and they are publicly available to all stakeholders. Additional information, however, could be gleaned from provider or MCE contracts, additional policy documents, or from an understanding of how regulations are enforced, or not, in practice. Another limitation is that the summaries reflect state law at a single point in time. Statutes and regulations are amended on an ongoing basis. This means that, at the point of publication of this Compendium, some statutes and regulations will have been amended, repealed, or replaced, rendering some portion of the summaries no longer accurate.[15] Last, because data collection requires deliberate selection of some characteristics over others and some components of regulatory oversight (such as building, fire, and zoning requirements) were not included, the scope of these summaries cannot be considered exhaustive.
| FIGURE 1. Domains and Subdomains of Oversight and Operation of Residential Treatment Facilities |
|---|
 |
Organization of the Report
Section 2 provides an overview of state regulatory provisions covering the two broad domains and 14 subdomains introduced in the study framework, including primary implications of those findings. Section 3 contains an overview of state Medicaid funding for services furnished in these settings and related policies, including primary implications of those findings. Section 4 discusses the key trends identified in this Compendium, including discussion of the ways in which state licensing regulations and Medicaid requirements often complement each other. Appendix A includes detailed tables showing results in each subdomain by state, and Appendix B contains links to each of the individual state licensing and Medicaid summaries. Appendix C contains a more complete methodology than that in Section 1 of this Compendium.
SECTION 2. OVERVIEW OF THE NONMEDICAID RESIDENTIAL TREATMENT REGULATIONS
The two primary domains examined relate to: (1) regulatory standards regarding processes of oversight such as regulation and licensure; and (2) regulatory standards regarding facility operation that are conditions of operation and licensure. Each domain and subdomain (hereinafter domains) is addressed in turn below. We provide an explanation for why each domain is important to the regulation and oversight of residential treatment, what each domain encompasses, and a discussion of major findings.
Domains Regarding Processes of Oversight
Domains regarding processes of oversight include categorization of regulated facilities, identification of unregulated facilities, state agency responsibility for oversight, processes of licensure and basic oversight, and processes of ongoing oversight.
| FIGURE 2. Categories of Regulated Residential Treatment Facilities |
|---|
 |
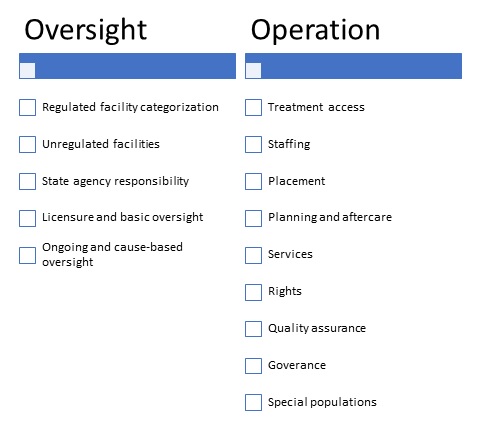
Categorization of regulated facilities. State regulations identify residential treatment facilities in many ways. Those identified in the regulations, therefore, had to be categorized in order to understand and describe the scope of what is regulated in a given state. We began with a distinction between mental disorder and SUD treatment facilities, given the historic bifurcation of the two systems,[16] and with an understanding that some states would distinguish facilities on the basis of their sources of funding. Further categorization was not possible until after data collection, and this post hoc categorization was primarily intended to identify major categories of residential treatment as often viewed by the states. Figure 2 depicts the categories ultimately used.
We discuss separately below the categorization for regulated mental disorder and SUD residential treatment, as well as categorization by funding source. It is apparent that the landscape of regulated residential treatment in the states is as diverse as the states themselves. There are many differences among states, as further discussed below.
-
Mental disorder residential treatment. The largest group of mental disorder residential facility types were those labeled as some form of specialized crisis facility. At least 32 states have such facilities serving individuals with mental disorders, some of which also serve clients with SUDs.[17] Detail by state is included in Table A1 and in the relevant state summaries (Appendix B). In addition to the states that regulate crisis facilities as such, some simply incorporate crisis services into other types of residential facilities. A much smaller number of states regulate facilities within the other identified categories. Nine states included facilities labeled as either short-term or transitional. The time period covered by this label varies considerably (e.g., 90 days or less for short-term facilities in Florida vs. 12 months for transitional facilities in California).[18, 19] Six states expressly label mental health facilities as long-term and, again, what is considered long-term varies by state (e.g., 60 days or greater average length of stay in Florida vs. 18 months maximum in California).[20, 21] Three states label or define certain facilities as intensive. An example of an intensive mental disorder residential treatment facility is the Minnesota Intensive Residential Treatment Services (IRTS).[22] In addition to states with facilities specific to women, which are addressed in the section of this Compendium regarding special populations, at least three states have facilities focused on specific populations. One example is Virginia, which has separate regulations specific to acute gero-psychiatric residential services.[23] A similarly small number of states identify residential facilities for individuals with specific conditions, in particular, three for eating disorders.[24] Finally, at least 31 states identify residential mental disorder treatment with nonspecific labels that do not fit our categories (e.g., Mental Health Centers, Residential Treatment Programs, Specialized Treatment Facilities). In addition, four states that do not identify any regulated residential mental disorder treatment facility types that fall within the definition used in this study.
-
Substance use disorder residential treatment. States also take many approaches to labeling, defining, and categorizing residential SUD treatment facilities. As with mental disorder facilities, crisis facilities often are so labeled (13 states), although it is clear that withdrawal management and other facilities also handle individuals presenting with high acuity. As noted above, some states have crisis facilities that are not strictly limited to mental disorder versus SUD treatment. Additionally, 35 states have SUD treatment labels that defy categorization (e.g., Specialized Treatment Facilities).[25] Facilities also were categorized as follows (see Table A2 for more detail by state):
-
States that expressly identify by label or definition the ASAM level applicable to a specific facility type, which we include if they were identified as being residential. These are Levels 3.1 (16 states), 3.2-WM (13 states), 3.3 (ten states), 3.5 (15 states), 3.7 (ten states), and 3.7-WM (12 states).
-
States may identify facilities as low, medium, or high-intensity, with or without parroting the ASAM label or level number. In some instances,[26] a state may reference ASAM with regard to these facilities, but not expressly link by level. In those instances, for purposes of the Appendix, we did not attempt to draw that connection. Rather, we relied on the state's designation as low, medium, or high. Whether identified using a precise ASAM label (e.g., Clinically Managed Low-Intensity Residential Services) or another label of low, medium, or high, 16, nine, and 16 states, respectively, fell into these categories. In some instances, states identify Level 3.3 with medium-intensity services for adults,[27] although that is inconsistent with the current ASAM criteria and reflects the older criteria.[28] In those instances, we counted the state as providing Level 3.3 services (because that is how they are identified by the state) and medium-intensity services.
-
Fourteen, 15, and five states identify detoxification/withdrawal management facilities as Clinically Managed, Medically Monitored, or Medically Managed, respectively, in accordance with ASAM criteria. Ten states identify some withdrawal management facilities as social detoxification. In some cases, social detoxification is expressly linked to ASAM Level 3.2-WM or to Clinically Managed Detoxification,[29] in which case we included it in both categories. Some states may use the term medical detoxification or medically supervised detoxification, without clear indication whether it is medically monitored or medically managed. In those instances, we included it with other unspecified withdrawal management as Detoxification/Withdrawal management.[30] A total of 23 states have facilities that we have placed into the general Detoxification/Withdrawal management category.
-
Transitional, short-term, and long-term are labels that states sometimes use to identify facilities and, when that is the case, we counted the categories accordingly, with 11 states using the label transitional, five states the label short-term, and six states the label long-term.
-
-
Funding criteria. In many states, regulations and/or licensing requirements vary on the basis of a facility's sources of funding. Differential regulation and/or licensure based on funding relates to whether a facility receives public funds (including block grant funds, state financing, and/or Medicaid). In Table 1, we identify the number of states that indicate requirements applicable to both Medicaid and other public funds in their regulations and licensure requirements. Separate requirements related only to Medicaid are discussed in our review of Medicaid regulations (see Section 3).
| TABLE 1. Number of States Regulated and Licensed by Funding Source | ||
|---|---|---|
| Requirements | Mental Health | Substance Use |
| Regulated based on funding source | 18 | 22 |
| Licensure based on funding source | 16 | 17 |
| NOTE: Detailed in Table A3 and Table A4. This table does not include information about requirements applicable only to Medicaid. | ||
One example of a state with multiple approaches to regulation is Ohio. Licensure by the Ohio Department of Mental Health and Addiction Services is required for all residential mental health facilities.[31] Separate certification by the Department also is required if the facility provides services that are funded by: (a) the Ohio Medicaid program for community mental health or community addiction services; (b) a board of alcohol, drug addiction, and mental health services; or (c) federal or department block grant funding for certified services. In addition, other Ohio facilities may voluntarily request certification.[32]
It is important to note that regulations and licensure are not the only mechanisms that a state has to oversee publicly-funded facilities. Of the states counted in Table 1, the regulations based on funding often coexist with other regulations for a larger group of residential facilities. For the subset of facilities receiving block grant funds from the state, oversight also or alternatively may occur pursuant to contractual provisions.
Identification of unregulated facilities. After categorizing types of facilities that are regulated, we undertook to determine which facilities in the states are unregulated. This is important in order to understand areas where state oversight and regulation are not currently present. Doing so requires a thorough understanding of what is regulated. From that, one can conclude that certain facility types are unregulated. Beyond that, unless there is a clear understanding of the types of facilities that actually exist in a state, it is impossible to say that a given state contains specific types of unregulated facilities. However, states may use other levers of oversight such as legally binding contracts for facilities receiving state funds.
Our survey of the states found that residential mental disorder treatment facilities are less likely to be regulated and/or licensed than are residential SUD treatment facilities. Table A5 in the Appendix identifies states by whether they have regulation and/or licensure of every type of mental disorder or SUD residential treatment that is within the scope of this study. We estimated that 23 states have fully regulated all residential mental disorder treatment in their jurisdiction and that 39 states have fully regulated all residential SUD treatment. Of those states included in Table A5 as not fully regulating the range of residential treatment in the state, it is important to note that most, in fact, do regulate a segment of residential treatment. The following are some examples of situations in which states are classified as having unregulated or potentially unregulated facilities:
-
A state may have no licensure regulations regarding mental disorder residential facilities.[33]
-
A state may regulate or license only facilities receiving public funding, although, in some instances, private facilities may seek licensure voluntarily.[34]
-
A state may regulate a limited range of facility types, and it is impossible to determine whether there actually are any such unidentified, unregulated facilities. An example is a state where regulated residential mental disorder treatment consists of two facility types that can also provide SUD treatment, Acute Crisis Units, and Therapeutic Communities.[35] In this instance, it is possible that those two types of facilities encompass every type of residential mental disorder treatment in the state, or they may not.
-
A state may have agency staff who indicate that certain types of facilities exist but are unregulated. An example is a state in which agency staff indicated that residential mental health facilities of less than five beds are not regulated.[36]
State agency responsibility. The state agency responsibility for M/SUD oversight varies widely between states, with variability according to agency focus (either mental disorder treatment, SUD treatment, or both) as well as according to how the state assigns responsibility for regulation and licensure across different agencies. Table A6 in the appendix captures the current state of separate versus combined agency oversight. States are increasingly integrating all functions into a single agency (40 states), although many still use distinct subagencies for oversight of different types of residential treatment. Other states still administer the functions of regulation and licensure across multiple agencies according to the unique structures of the M/SUD treatment systems and public health tradition in the state. Among the latter were 12 states with agencies specifically regulating residential mental disorder treatment and 15 states doing so for residential SUD treatment. A few states had some variation on this approach to regulation. Georgia, for example has one agency regulating both with additional regulation by another agency for SUD. Kentucky, New Jersey, and Vermont have both combined and separate agencies with regulatory responsibility. We refer the reader to the state summaries (Appendix B) for further details regarding individual states.
Processes of licensure and basic oversight. The licensure process can be quite complex and entail many requirements. This may include requirements imposed through multiple processes. Thus, the licensure process may entail, for a single facility, multiple applications or processes with one or more agencies. This may apply, for instance, if a facility must be separately licensed to operate and certified to obtain public funding. In the first two rows of Table 2, we identify when this complication exists. One example is Colorado, where the Department of Human Services, Office of Behavioral Health requires designation for mental health facilities that receive public funds or that initiate an involuntary hold on a person with mental illness. This includes, among other facilities, Acute Treatment Units, which also must be licensed by the Colorado Department of Public Health and Environment.[37]
| TABLE 2. Number of States Using Different Approaches to Licensure and Other Oversight | ||||
|---|---|---|---|---|
| Requirements | Mental Health | Partiallya for Mental Health |
Substance Use | Partiallya for Substance Use |
| One licensure/certification (L/C) | 38 | 0 | 41 | 1 |
| Multiple L/C | 7 | 0 | 8 | 1 |
| Duration identified | 45 | n/a | 50 | n/a |
| Inspection at L/C | 41 | 2 | 42 | 6 |
| Accreditation required | 7 | 2 | 3 | 9 |
| Deemed status | 14 | 7 | 23 | 8 |
| CON required | 10 | 7 | 4 | 11 |
NOTE: Detailed in Table A7 and Table A8.
|
||||
The remainder of Table 2 indicates the extent to which licensure processes offer potential for state assessment and/or oversight of facility operations and quality. To that end, we focused on four components. These include: (1) the duration of licensure, because that may affect how often facilities are examined by the state; (2) whether an inspection or survey is required at licensure; (3) whether states require accreditation by an outside entity and, if not, whether accreditation serves to offset some portion of the requirements for licensure; and (4) whether a certificate of need (CON) is required.[38] Requirements for a CON typically are found in state law and historically have been used to ensure that operation of a proposed new facility meets the needs of the community.
The duration of licensure for residential treatment varies but is specified in more than four-fifths of states (Table 2). In many states, a renewal application must be submitted annually; in a few others, the duration may be as long as 3 years.[39] Some states provide a time range during which expiration may occur. For example, Kansas regulations state that the duration is "a term to be stated upon the license, which shall not exceed two years, unless revoked earlier for cause."[40] More detail regarding the duration of licensure by state is included in Table A7 and Table A8.
Most states require an inspection or survey to be completed as part of licensure (Table 2), although some regulations appear to include agency discretion (e.g., for SUD residential treatment licensure in Texas, "If an on-site inspection is necessary, the Commission will conduct the inspection within 45 days of receiving a materially complete application packet").[41] In total, 43 and 48 states clearly require licensure inspection for mental disorder and SUD residential treatment, respectively, either fully or partially for all such facilities.
In addition to licensure, accreditation by an independent accrediting body such as TJC, the Commission on Accreditation for Rehabilitative Facilities, or the COA may be required. An actual regulatory requirement is relatively uncommon for residential treatment facilities, with 9 (mental health) and 12 (SUD) states requiring for either some or all residential facilities. Such requirements, however, may be imposed by contract, as is true in New Hampshire.[42] One example of a state where accreditation is required by regulation is Nebraska, where locked mental health facilities or facilities that use mechanical or chemical restraints or seclusion must be accredited.[43] It is more common that regulations convey "deemed status" on facilities that achieve accreditation, allowing accreditation to supplant aspects of licensure (21 [mental health] and 31 [SUD] states). For example, in Missouri, accreditation by an approved body confers deemed status, allowing an applicant for certification to submit a different application and forego a survey, other than to clarify aspects of the accreditation.[44] As another example, in Utah, the licensing agency may rely on the accreditation documentation to assist in determining if licensure is appropriate.[45] When accreditation replaces part of the licensing process, it often takes the place of inspections, although states nearly always reserve the right to conduct inspections for cause.[46]
Some states also may require a CON before a facility may be built or opened, although this is only approximately one-quarter of states for some or all facility types. This does vary by facility type, as, for example, in Florida, where a CON is required for Crisis Stabilization Units and Short-Term Residential Treatment Programs.[47] Alternatively, states may require a demonstration of need so as to obtain licensure, apart from any formal state CON requirements that may exist.[48]
Ongoing oversight. Ongoing facility oversight by state regulators, licensing bodies, or their surrogates takes different forms, providing additional opportunities for state agencies to assess facility compliance and quality. In Table 3, we identify the number of states that require: (1) regular ongoing inspections; and (2) cause-based inspections. License renewal, which typically happens at regular intervals, provides an opportunity for review of a renewal application, document review, and for renewal site inspections. Approximately four-fifths of states clearly provide for renewal inspections. States often explicitly also provide for cause-based inspections or other investigations, which may be prompted by various events, and for unannounced inspections. Among the states, approximately four-fifths have regulatory requirements mentioning such inspections. Within these requirements for routine ongoing or cause-based inspections, there are occasional nuances. One example is Texas, where the Health and Human Services Commission "may conduct a scheduled or unannounced inspection," but where it is not clearly specified in the regulation that routine inspections will regularly be required for licensure or renewal.[49]
| TABLE 3. Number of States with Requirements for Ongoing or Cause-Based Inspections | ||||
|---|---|---|---|---|
| Requirements | Mental Health | Partiallya for Mental Health |
Substance Use | Partiallya for Substance Use |
| Ongoing inspections | 42 | 2 | 43 | 4 |
| Caused-based inspections | 40 | 1 | 44 | 1 |
NOTE: Detailed in Table A9.
|
||||
State laws also generally provide for required plans of correction and action pursuant to those plans; actions against the license such as limitation, suspension, or revocation; and/or penalties (see Appendix B for details by state).[50] In addition, states may rely on contractual provisions for entities receiving public funding through block grants, Medicaid, or other avenues to activate oversight at times other than upon renewal. Thus, even if provisions were not located in the licensing regulations regarding ongoing or cause-based inspections, it is very possible that such requirements exist in other formats.
Domains Regarding Facility Operations
Domains regarding facility operations include standards regarding access to treatment, staffing, placement, treatment and discharge planning and aftercare, treatment services provided (including medication-assisted treatment [MAT]), service recipient rights, quality assurance or improvement, governance, and requirements related to special populations.
Access to treatment. Access to the full continuum of behavioral health treatment is a persistent problem and multiple barriers to accessing care may exist. Regarding access to residential treatment, this study examines whether states impose requirements regarding wait time to access treatment. This was selected as a discrete measure of whether access is explicitly addressed in the regulations. About a third of the states have wait times or requirements regarding wait time facility policies present in the regulations (15 [mental health] and 17 [SUD], partially or fully) (see Table 4). Where such requirements exist in the regulations, they may appear as a general mandate[51] or as applicable to certain facility types only (e.g., South Carolina crisis stabilization units or Idaho withdrawal management).[52, 53] A different approach is taken by Missouri; its regulations include what are called "Essential Principles" that are intended to guide the facility. Among the Essential Principles is "Easy and Timely Access to Services," in which the Department of Mental Health suggests (but does not require) that some potential performance indicators for mental health services generally might include: (1) same-day access to services; or (2) reduced wait time to set a first or subsequent appointment(s).[54] There also are instances in which wait time requirements are applied through nonregulatory means. For instance, staff from both Arizona and Tennessee indicated that they have online portals to manage wait times. Although these are not included as regulatory requirements, they do exist and are addressed in the respective state summaries (Appendix B). Several states have wait time requirements specific to priority populations, which is discussed further under Special Populations. We also discuss, under Treatment Services, regulatory requirements that access not be denied because a person is receiving or has received MAT or, in the case of mental health facilities, has an SUD.
| TABLE 4. Number of States with Regulatory Provisions Regarding Wait Times | ||||
|---|---|---|---|---|
| Requirements | Mental Health | Partiallya for Mental Health |
Substance Use | Partiallya for Substance Use |
| Wait times | 9 | 6 | 8 | 9 |
NOTE: Detailed in Table A10.
|
||||
Staffing standards. Qualified staff at all levels are important to the provision of quality care in residential treatment. Many states include explicit staffing requirements in regulations,[55, 56] whereas other states may rely more heavily on incorporation by reference, such as of ASAM staffing standards for SUD residential treatment, which Iowa staff indicate are applicable,[57] or, perhaps, on requirements placed in policy documents or contracts. For this study, staffing was examined from two perspectives: (1) regulatory requirements related to required staffing, credential or experience requirements, and required levels for staffing; and (2) regulatory requirements regarding staff training.
The focus for the first was on quantifiable standards, such as whether there are any requirements related to facility administrators, medical directors, other medical staff, clinical staff, or direct care staff, and the extent to which staffing ratios or other criteria for staffing levels exist (Table 5). States may approach this as simply, for instance, requiring that there be an administrator, or, instead, may specify acceptable age, educational credentials, and/or experience. Mental health residential facility regulations are somewhat less likely than SUD regulations to have administrator requirements. States are much less likely to require that facilities have a medical director and are even less likely to require that to be a physician.[58] Within the realm of residential SUD treatment, requirements for a medical director or even medical staff were most common in residential detoxification or withdrawal management facilities as opposed to other types of residential treatment.[59] Requirements related to clinical staff refer to licensed mental disorder or SUD treatment providers such as psychologists, social workers, or drug and alcohol dependence counselors. Among the states requiring that substance abuse counseling generally be provided by licensed drug and alcohol dependence counselors are a few that expressly except from that requirement otherwise licensed professionals such as physicians or psychologists.[60] Direct care staff, as that term is used in this Compendium, means nonlicensed staff, or peer staff who may be certified, who are charged with day-to-day contact with residents. In all instances, SUD regulations are more likely to specify such staffing requirements.
| TABLE 5. Number of States by Staffing Standards for Licensure | ||||
|---|---|---|---|---|
| Requirements | Mental Health | Partiallya for Mental Health |
Substance Use | Partiallya for Substance Use |
| Standards | ||||
| Administrator | 32 | 5 | 34 | 6 |
| Medical Director | 7 | 4 | 7 | 12 |
| Medical staff | 23 | 9 | 20 | 24 |
| Clinical staff | 3 | 2 | 37 | 10 |
| Direct care staff | 30 | 4 | 31 | 6 |
| Staffing levels | ||||
| Ratios | 18 | 9 | 17 | 17 |
| Adequate | 26 | 4 | 31 | 10 |
NOTE: Detailed in Table A10, Table A11, Table A12.
|
||||
We also examined the extent to which states incorporate staffing ratios or requirements for policies regarding ratios into regulations and/or require that there be "sufficient" or "adequate" staffing. In some instances, a state may use both approaches, often depending on facility type.[61, 62] When ratios are prescribed, it typically is for certain types of personnel and not others (e.g., nursing staff, clinical staff, direct care staff). Again, this is somewhat more likely to be seen in SUD regulations than in those governing mental health residential facilities. It also is likely that states without explicit ratios in regulations do include them in other policy documents or contracts.
For the second aspect of staffing, we looked at orientation and ongoing training requirements, as well as two selected potential foci of training, specifically staff training regarding trauma-informed care and regarding suicide assessment and/or prevention (or crisis intervention). Table 6 provides basic information on training standards that are incorporated into state regulations. Training requirements vary greatly. Some are specific as to orientation versus ongoing training, whereas others are not explicit about the timing for training. Some state regulations go into great detail about mandatory or optional training required of staff generally, in contrast to others that focus on training for specific staff types. Some, such as regulations governing personnel in residential mental health facilities in Iowa, vary the training requirements by level of care, for example, placing greater emphasis on training for staff at Intermediate Care Facilities for Persons with Mental Illness[63] than at Residential Care Facilities with a Three to Five-Bed Specialized License.[64]
States have many different areas on which they may elect to focus staff training. Training subjects range from first aid to dual diagnosis to restraint and seclusion (R/S), with many other topics emphasized by different states. More than four-fifths of states use regulations as a way to impose training requirements. The training requirements are highlighted in Table 6; training regarding trauma-informed care and regarding suicide assessment and/or prevention, are just two out of many possible subjects of regulation-mandated training. They were selected, however, because trauma-informed care is generally regarded as a best practice in both mental disorder and SUD treatment and because training related to suicide was selected as an indicator of focus on safety. More states require use of trauma-informed care, sometimes in conjunction with other requirements that staff be "qualified" to perform their job responsibilities, than do states that explicitly require staff training in trauma-informed treatment. One example of the former is Mississippi, which requires that all services be designed to provide trauma-informed care but does not include a specific regulatory requirement related to training in such care.[65] Similarly, although crisis services may be a fundamental part of the treatment spectrum in many states or suicide assessment explicitly must be conducted, not all state regulations are explicit in requiring more general suicide assessment and prevention training for staff. An example is Missouri, which requires suicide screening as part of admission assessment, "competent staff" to identify risks and behaviors that can lead to a crisis and the use of "effective strategies to prevent or intervene," the development of crisis prevention plans where at-risk behavior including suicide is identified, and "ready access to crisis assistance and intervention ... provided by qualified staff," but does not include an explicit requirement for suicide prevention and assessment training.[66] We include in Table 6 only those states that are explicit about requiring trauma or suicide-related (or crisis-related) training in regulations.
| TABLE 6. Number of States by Training Requirements for Licensure | ||||
|---|---|---|---|---|
| Requirements | Mental Health | Partiallya for Mental Health |
Substance Use | Partiallya for Substance Use |
| Orientation and/or ongoing training | 31 | 10 | 36 | 11 |
| Trauma-informed care training | 4 | 0 | 5 | 1 |
| Suicide assessment/prevention training | 6 | 2 | 4 | 3 |
NOTE: Detailed in Table A13.
|
||||
Staffing in residential care is one of the few domains that was explicitly addressed in earlier research. Our scan found much lower rates of required training than was found in data from two short reports by the SAMHSA. SAMHSA examined this subject for mental disorder and SUD specialty treatment, using 2010 N-MHSS and 2013 N-SSATS data.[67] Those analyses examined three markers of quality assurance practices related to facility workforce. Practices varied considerably by state and by type of organization (e.g., private for-profit, private nonprofit, state government entities, Veterans Health Administration). Table 7, however, shows the results for the three measures in residential treatment settings for mental health and SUD respectively.
These measures reflect the data available from the surveys, which are voluntarily reported, but generally indicate that large numbers of the residential facilities surveyed followed these practices. These are not comparable to the data collected as part of this study, which relate to requirements found in state statutes and regulations and include neither facility-required training nor requirements imposed by nonregulatory sources. Nonetheless, even state statutes and regulations frequently include training requirements. These studies, however, highlight the widespread use of two practices that should be a basic part of treatment delivery, in particular, continuing education and regular case review with a supervisor, and a third less commonly used practice of case review by a quality review committee.
Placement standards. Placement in the appropriate setting and level of care is important to ensure that patients receive the care they need. For example, research shows that receiving SUD treatment in the appropriate type and intensity of care can positively affect treatment participation and retention, reduce use of more intensive services, and result in better outcomes than is true for those placed in a lower or, in some instances, a higher level of care than is recommended[68] by the ASAM Patient Placement Criteria.
To determine whether state placement oversight exists, we examined whether there were specific criteria for placement and/or assessment, including whether regulations delegated this function by way of facility policy and procedure requirements. Within the realm of SUD treatment, we looked at regulatory requirements related to use of the ASAM Patient Placement Criteria. Also included in the state summaries (Appendix B) are requirements regarding continued placement and discharge criteria.
Placement standards within state licensing regulations generally fall into four categories, more than one of which may be present in any given state:
-
Specific statements in the law about the population intended to be served by a given facility type.[69]
-
Requirements that facilities have policies or procedures setting forth requirements for and/or approaches to admission and determining if placement is appropriate.[70]
-
Specific requirements for how appropriate placement is determined and, sometimes, by whom, such as in New Hampshire residential SUD treatment facilities where, among other things, requirements include "a screening and assessment interview conducted or supervised by a licensed counselor to determine ... that the client meets the requirements for treatment of a substance use disorder; and ... a determination of the appropriate ASAM level of care needed."[71] This also may be determined by role rather than by credential, such as in Idaho where the Department of Health and Welfare determines whether an individual is eligible for Crisis Intervention Services.[72]
-
Criteria or requirements for policies for continuing stay or discharge, such as Montana standards for chemical dependency facilities that require use of the ASAM Patient Placement Criteria to establish level of care for, in addition to placement, continued stay, discharge criteria, and ongoing assessment of the client.[73]
If any regulatory specificity is provided about population served or how to ascertain appropriateness, the analysis considers that specific placement criteria do exist. We identified these criteria for 33 (mental disorder) and 45 (SUD) states partially or fully (Table 8). We also treat regulations as requiring a screening or assessment for placement if it is clear that a placement assessment is required, for some or all facility types, either before admission (23 states and 31 states, respectively, for mental disorder and SUD residential treatment) or within 24 hours of admission (33 and 48 states, respectively for mental disorder and SUD residential treatment). In some instances, early assessments are required, but regulations do not clearly indicate that it is part of placement determination; in those instances, we treat that as an "other" nonplacement assessment if required within 24 hours. Many states have additional requirements for ongoing assessments later in the early course of treatment, which we do not include in this study. For example, the Minnesota variance for IRTS requires that the LOCUS be used for assessment of suitability for the setting, to be conducted within 10 days of admission.[74]
If regulations require use of the ASAM Patient Placement Criteria for SUD treatment level of care determination, or if state staff so indicated, we specifically included that. Thirty-six states were identified as relying on the ASAM criteria for placement in SUD residential treatment. This excludes other states that may require it as part of Medicaid regulations, through policy documents, or by contract. In contrast, although an assessment may be required, it is uncommon for state regulations to indicate a specific tool for admission to residential mental disorder treatment. Among the rare instances in which a regulation approached doing so was in Utah, where service providers who contract with the Division of Substance Abuse and Mental Health and County Local Authority programs are subject to regulations that require levels of care to be "based on the ASAM or equivalent Mental Health criteria."[75]
| TABLE 8. Number of States Regulating Placement Criteria | ||||
|---|---|---|---|---|
| Requirements | Mental Health | Partiallya for Mental Health |
Substance Use | Partiallya for Substance Use |
| Criteria for placement | ||||
| Specified in regulations | 26 | 7 | 38 | 7 |
| Facility policy required | 17 | 1 | 30 | 3 |
| Placement assessment | 31 | 2 | 44 | 4 |
| ASAM for placement | 1 | 1 | 23 | 13 |
| Timing of assessment | ||||
| Before admission for placement | 18 | 5 | 23 | 8 |
| Within 24 hours for placement | 5 | 1 | 5 | 7 |
| Within 24 hours nonplacement assessment | 9 | 3 | 9 | 8 |
NOTE: Detailed in Table A14 and Table A15.
|
||||
Treatment and discharge planning and aftercare requirements. Treatment planning and regular review of treatment plans are critical to ensure that appropriate treatment is in place, delivered, and adjusted when required. In addition, discharge or aftercare planning is important to determine whether the treatment plan and delivery are pointed in the intended direction, working toward objectives of recovery and ongoing treatment outside of the residential setting. In addition to examining these requirements, we also analyzed whether states had in place provisions related to residential delivery of aftercare or follow-up, in the interest of continuity of care and avoiding loss to treatment.
Most state regulatory structures include a requirement for treatment or service planning; we located 44 and 48 states with such regulatory requirements applied to mental disorder and SUD residential treatment, respectively, either partially or fully (Table 9). It is more common that states fail to include such a requirement in very short-term services such as Vermont's residential and withdrawal management SUD treatment if a person is present fewer than 6 days.[76] It also is common to see requirements for time to completion and timing of review, although we identified them more frequently in regulations pertinent to SUD residential treatment than mental health. These requirements are generally specific but, in some instances, may be requirements that must only be established in policies or procedures by the facility or, for timing of review, as required in the individual's treatment plan.
Discharge planning often is required (by more than 60% of states and more so for residential SUD treatment), sometimes as early as upon admission, such as for Illinois' Crisis Stabilization Units.[77] Discharge planning also is often referred to as aftercare planning. In a very few instances, however, aftercare actually may encompass provision for contact with the client after discharge, such as following residential SUD treatment,[78] or, less commonly, a clear option for ongoing aftercare by a residential SUD treatment facility.[79]
| TABLE 9. Number of States with Requirements Regarding Treatment or Discharge Planning or Aftercare Services | ||||
|---|---|---|---|---|
| Requirements | Mental Health | Partiallya for Mental Health |
Substance Use | Partiallya for Substance Use |
| Treatment plan required | 42 | 2 | 43 | 5 |
| Timeframe to complete | 26 | 8 | 30 | 10 |
| Timeframe to review | 30 | 5 | 28 | 14 |
| Discharge plan required | 32 | 5 | 42 | 4 |
| At admission or shortly thereafter | 13 | 7 | 13 | 8 |
| Aftercare services/follow-up required | 2 | 3 | 6 | 5 |
NOTE: Detailed in Table A16 and Table A17.
|
||||
Treatment services. Ensuring the provision of evidence-based or best practice treatment is crucial to maintaining high-quality residential services for M/SUDs. Given the range of types and levels of treatment, we focused on whether therapeutic services were required by the regulations, if amount was specified, and whether states included requirements regarding evidence-based or best practice treatment. One specific evidence-based practice, examined within the realm of service delivery, was medication treatment as part of MAT specific to residential settings,[80] discussed in greater detail below.
Because we excluded residential facilities that do not provide clinical treatment (excepting some withdrawal management facilities), most residential treatment facility regulations did include at least some reference to services to be provided, including clinical services (Table 10). Whenever regulations mandated some form of clinical treatment, even if only referencing "treatment," "counseling," "psychological," or "therapeutic" services or, in the case of withdrawal management, nursing services, we considered that the state had service requirements specific to clinical service types. When regulations specify the number of hours of clinical treatment, that is indicated separately because it is less commonly included in regulations and more likely to be in a policy or contractual document. In all instances, these requirements were most commonly found in regulations applicable to residential SUD treatment than to residential mental disorder treatment.
To determine whether evidence-based or best-practice requirements were in place, we included states where "evidence-based" practices or "best practice" were required by the regulations. For example, the Colorado Office of Behavioral Health regulations require that a "best practice" comprehensive assessment be used for both M/SUD residential treatment at placement[81] and that "evidence-based" practices be used in crisis stabilization units.[82] We also included states where trauma-informed care,[83] motivational interviewing,[84] or MAT[85] is explicitly required to be used or, in the case of the last, available, although these requirements may vary by facility type within states. We identified such regulatory requirements for 11 (mental health) and 26 (SUD) states, partially or fully. We recognize that there are other evidence-based treatments, but we selected these as representative approaches that are most likely to be reflected in regulatory language.
| TABLE 10. Number of States with Regulations Regarding Services | ||||
|---|---|---|---|---|
| Requirements | Mental Health | Partiallya for Mental Health |
Substance Use | Partiallya for Substance Use |
| Any service requirements | 45 | 1 | 51 | 0 |
| Specific to clinical service types | 33 | 6 | 41 | 6 |
| Specific to clinical service hours | 5 | 5 | 9 | 17 |
| Evidence-based | 9 | 2 | 11 | 15 |
NOTE: Detailed in Table A18.
|
||||
Given the importance of MAT as an evidence-based treatment for opioid use disorder (OUD) and alcohol use disorder (AUD), additional attention was paid to the incorporation of requirements for MAT into regulations specific to residential treatment. Medications for OUD include methadone, buprenorphine, and naltrexone and for AUD include naltrexone, acamprosate, and disulfiram.[86]
Table 11 identifies the states that have explicit requirements for residential treatment related to receipt of MAT services. Only about a third of the states require it for SUD residential treatment, and only a fraction for mental health facilities. State regulations may expressly allow or require MAT to be offered or access to it provided (18 states for SUD, fully or partially), may prevent providers from denying access to SUD treatment because a person is receiving MAT (eight states for SUD, fully or partially), or may establish a right to receive or be offered MAT (ten states for SUD, fully or partially). One approach is to allow a residential provider to offer MAT if it is suitably licensed.[87, 88] Some states explicitly require MAT in residential detoxification or withdrawal management facilities,[89] and some require the provision of medication in such facilities but are not specific about it being MAT (e.g., "medication should be available to manage withdrawal/intoxication from all classes of abusable drugs").[90] States also may require that residential or other SUD providers not discriminate against[91] or deny services to[92] an individual because he or she is receiving MAT. In Utah, all service providers contracting with the Division of Substance Abuse and Mental Health and all County Local Authority programs must provide written information to every treatment participant regarding rights to MAT[93] and, in community-based treatment programs, all individuals with AUD and/or OUD must be educated and screened for the potential use of MAT.[94]
| TABLE 11. Number of States with Regulations Regarding MAT Specific to Residential Treatment | ||||
|---|---|---|---|---|
| Requirements | Mental Health | Partiallya for Mental Health |
Substance Use | Partiallya for Substance Use |
| Requirements for MAT services | 1 | 1 | 6 | 12 |
| MAT and access to SUD treatment | 1 | 1 | 5 | 3 |
| Rights to MAT in residential treatment | 2 | 0 | 6 | 5 |
NOTE: Detailed in Table A19.
|
||||
Service recipient rights. Statutes and regulations governing service recipient or patient rights evolved out of a history of maltreatment in some institutions. The range of rights is broad and varies across states. For that reason, in addition to identifying if rights of any sort were memorialized by law, we selected two discrete aspects of service recipient rights for quantification. These related to: (1) the right to voice grievances, taken as an indicator of the ability of service recipients to enforce their rights in general; and (2) rights related to restraint and seclusion, because restraint and seclusion affect both safety and dignity. We examine above the express right to receive MAT in residential treatment.
Service recipient rights may include the right to informed consent, privacy, communication, to be treated with dignity, to be treated in the least restrictive appropriate setting, and to be free from abuse, neglect, or exploitation, among many other frequently enumerated rights for individuals in the M/SUD treatment system. In Table 12, we indicate whether any such rights were located that were applicable to residential treatment within the states. Laws regarding service recipient rights were identified in 42 and 45 states, for mental disorder and SUD residential treatment.
The right to voice grievances is commonly found in state statutes and regulations and is indicative of the ability of service recipients to enforce their rights. We located such rights in 37 and 42 states, for mental disorder and SUD residential treatment, respectively, fully or partially. As an example, the state of New Hampshire relies on a statutory "Patients' Bill of Rights,"[95] which includes requirements that patients be "encouraged and assisted throughout the patient's stay to exercise the patient's rights as a patient and citizen. The patient may voice grievances and recommend changes in policies and services to facility staff or outside representatives free from restraint, interference, coercion, discrimination, or reprisal." States also may expand on statutory rights by regulation, for example, establishing procedures for submitting complaints or grievances and having them addressed and, occasionally, requiring that information on grievances be reported to the state.[96] Regulations requiring that grievances be reported to the state are not the norm, and some states do not, by regulation, require the reporting of grievances in residential SUD treatment but rather ensure service recipients of the general right to "contact the Department,"[97] placing the onus, at least in the regulations, on the recipient rather than on the provider.
Recipient rights related to restraint or seclusion reflect the fact that these behavior management techniques have repercussions both for safety and dignity. States take different approaches in their statutes and regulations regarding restraint and seclusion. These include: (1) no mention of these behavior management techniques in regulations; (2) prohibitions and/or restrictions on one or all of seclusion or physical, mechanical or chemical restraints; or (3) applying different requirements to different categories of facilities. One example of the latter two approaches is Indiana, which prohibits chemical restraints and allows physical restraint or seclusion only in Sub-acute Stabilization Facilities.[98] Regulatory requirements that restraint or seclusion be reported to the state are relatively uncommon, although they do appear, as for instance in Kansas regulations governing residential mental disorder treatment that require that it be reported if it "results in serious injury to the consumer."[99] As shown in Table 12, 42 (mental disorder) and 37 (SUD) states have some formalized rights regarding restraint or seclusion. It is completely prohibited in one state's mental health regulations and partially prohibited in another 18 states. It is completely prohibited in five state's SUD regulations and partially prohibited in 13 states. The majority of states that permit some form of restraint or seclusion have regulations regarding how they may occur.
| TABLE 12. Number of States with Regulations Regarding Service Recipient Rights | ||||
|---|---|---|---|---|
| Requirements | Mental Health | Partiallya for Mental Health |
Substance Use | Partiallya for Substance Use |
| Recipient Rights | 42 | 0 | 45 | 0 |
| Complaints/Grievances | 34 | 3 | 39 | 3 |
| Complaints reported to state | 2 | 6 | 4 | 7 |
| Rights re Restraint/Seclusion | 39 | 3 | 34 | 3 |
| Restraint/Seclusion Prohibited | 1 | 18 | 5 | 13 |
| Restraint/Seclusion Regulated | 24 | 16 | 17 | 12 |
| Restraint/Seclusion reported to state | 5 | 3 | 2 | 1 |
NOTE: Detailed in Table A20 and Table A21.
|
||||
Quality assurance or improvement. It is important to understand a wide range of aspects related to quality. For example, are there standards for high-quality safe treatment in place and is compliance with those standards monitored and enforced? To some extent, all the domains identified in this Compendium ultimately feed into quality. For purposes of examining quality assurance or improvement, specifically, we collected information on regulatory requirements for quality assurance or improvement plans, including whether some form of measurement was required to be integrated into those plans and whether either the plan or the results of implementation must be provided to the state.
Table 13 identifies the number of states with quality assurance/quality improvement (QA/QI) requirements within their regulations (37 [mental disorder] and 48 [SUD], partially or fully). Some states have explicit and very detailed requirements, such as Colorado, which requires that all facilities designated or licensed by the Office of Behavioral Health, or that contract with Office of Behavioral Health, have a program that monitors, evaluates, and initiates quality improvement activities. Among other things, this includes requirements for a written plan, quality measures of performance, documentation of quality improvement findings incorporated into clinical and organizational planning, and an annual evaluation that results in an update to the quality improvement plan as necessary. Colorado requires that the annual findings and report be available for review.[100] A few jurisdictions explicitly require data or plan submission (one [mental disorder] and 15 [SUD] partially or fully). For example, Minnesota requires that specific data related to residential mental disorder treatment facilities be submitted to the state and other data to the pertinent county.[101] In two states, facilities must undertake an assessment of need for residential SUD treatment.[102] Other states, such as Idaho, do not require quality assurance or performance improvement by regulation but do so, instead, under terms of contracts with entities receiving public funding.[103] All of these requirements are more abundant in the regulations governing residential SUD treatment than in the mental health regulations, including requirements for measurement as part of the plan.
| TABLE 13. Number of States with QA/QI Regulations | ||||
|---|---|---|---|---|
| Requirements | Mental Health | Partiallya for Mental Health |
Substance Use | Partiallya for Substance Use |
| QA/QI requirement | 34 | 3 | 46 | 2 |
| Written plan/policy | 27 | 3 | 38 | 2 |
| Needs assessment | 0 | 0 | 2 | 0 |
| Measurement | 19 | 7 | 26 | 7 |
| Provide to state | 0 | 1 | 5 | 10 |
NOTE: Detailed in Table A22.
|
||||
Governance standards. Facility governance concerns who is accountable for facility performance and safety and how they are tasked with responsibility. This study examined the extent to which states have some form of governance requirements in place. Many state licensing or oversight regulations include a requirement that facilities have a governing body or other entity responsible for facility governance or oversight. These requirements may be quite detailed in terms of matters the governing body must address.[104] Table 14 identifies the number of states in which requirements for governing bodies were located, with more than half of all states having regulations requiring this for mental disorder and SUD residential treatment. Although not included in this table, it is even more likely that state regulations will include requirements related to policies and procedures that effectively govern how the facility is operated. Those policies can touch on any or all aspects of factors explored in this Compendium (e.g., personnel, admission and discharge requirements, patient rights, quality assurance).
| TABLE 14. Number of States with Governing Body Regulations | ||||
|---|---|---|---|---|
| Requirements | Mental Health | Partiallya for Mental Health |
Substance Use | Partiallya for Substance Use |
| Governing body requirements | 30 | 6 | 38 | 3 |
NOTE: Detailed in Table A23.
|
||||
Special populations. States often focus on specific vulnerable populations to ensure that adequate services are available for them. To some extent, this reflects requirements for states to receive block grant funding, such as those for the SAMHSA Substance Abuse Block Grants regarding pregnant women and injection drug users.[105] Within the state summaries (Appendix B), we compile the different populations targeted, focusing in Table 15 on dual diagnosis, pregnant, and parenting women, and injection drug users, with a varied category of "other."
It is unusual for residential mental health facilities to be subject to regulations regarding provision of services to specific populations (Table 15). When there are such requirements, they tend to apply to facilities receiving public funds[106] and/or relate to individuals with a co-occurring SUD.[107] Regulatory requirements related to special populations most frequently apply to SUD treatment facilities. For such facilities, requirements related to individuals with dual diagnosis (29 states, partially or fully) or pregnant and parenting women (27 states, partially or fully) tend to be most frequently specified in the regulations. Some regulations also include requirements related to injection drug users (13 states, partially or fully). Specific requirements related to pregnant women or injection drug users in SUD treatment are generally attributable to federal block grant requirements and may exist in some states in regulations not examined as part of this licensure survey or may be in separate policy or contract documents, as is the case in Idaho, Texas, Vermont, and other states. In addition to the most frequently prioritized populations, other categories also appear in state regulations. A few salient examples, out of more than 20 special populations, include individuals with cognitive impairment due to substance use or co-occurring conditions,[108] those who have experienced traumatic events,[109] and individuals with a history of criminal justice involvement.[110]
| TABLE 15. Number of States with Regulations Regarding Special Populations | ||||
|---|---|---|---|---|
| Requirements | Mental Health | Partiallya for Mental Health |
Substance Use | Partiallya for Substance Use |
| Dual diagnosis | 9 | 6 | 27 | 2 |
| Pregnant and parenting women | 1 | 0 | 25 | 2 |
| Injection drug users | 0 | 0 | 11 | 2 |
| Other | 9 | 3 | 19 | 4 |
NOTE: Detailed in Table A24.
|
||||
SECTION 3. OVERVIEW OF STATE MEDICAID REQUIREMENTS FOR RESIDENTIAL TREATMENT
Medicaid is the largest payer of behavioral health services in the United States.[111] As such, regulation and oversight of Medicaid-enrolled providers by state Medicaid programs can have an outsized influence on the structure and quality of behavioral health treatment. Especially since CMS expanded the possibilities of Medicaid reimbursement for residential behavioral health treatment with the Section 1115 demonstrations, Section 1115 demonstration requirements have been seeping into the Medicaid regulations as well as into other state laws and regulations, including those pertaining to licensure. Hence, there is both an overlay of Medicaid with licensure requirements and influence by the Medicaid requirements on a broader range of programs. In addition, state Medicaid programs require that providers be licensed or certified in accordance with applicable laws in order to be enrolled in Medicaid. This has the effect of incorporating state licensure requirements into the Medicaid requirements, bolstering what Medicaid can expect of its providers.
As with the overview of nonMedicaid residential treatment regulations, as part of our review of Medicaid requirements we examined two domains, specifically: (1) standards regarding processes of oversight; and (2) standards regarding facility operation that are conditions of Medicaid enrollment and participation. Each domain and many of the subdomains addressed in Section 2 (hereinafter domains) is addressed in turn below, with explanation for why each domain is important to the regulation and oversight of Medicaid providers of residential treatment, what each domain encompasses, and a discussion of major findings. First, however, we examine the sources of state Medicaid authority to reimburse residential treatment.
In researching state Medicaid requirements, we primarily relied on state Medicaid regulations and Section 1115 demonstration documents, supplementing as necessary with additional sources. The relative absence of certain requirements in state Medicaid regulations, however, does not mean that Medicaid programs do not have service requirements in provider agreements with Medicaid or MCEs, provider manuals, or elsewhere. Similarly, some states may more passively rely on the presence of licensure requirements to ensure that service standards are in place.
Sources of State Medicaid Authority to Reimburse Residential Treatment
Historically, M/SUD treatment was not reimbursed as robustly as other medical care. Treatment relied heavily on public funding such as state and more local funding, as well as SAMHSA block grants. Requirements for reimbursement of M/SUD treatment were improved by the federal Mental Health Parity and Addiction Equity Act of 2008 and the 2010 Patient Protection and Affordable Care Act.[112] Insurance coverage for residential treatment, however, continued to be more restricted than was the case for community-based care.
Within Medicaid, these coverage restrictions stem from the Institution for Mental Disease (IMD) exclusion from reimbursement, which prevents the use of federal matching dollars for treatment in settings with more than 16 beds that primarily provide services to individuals with mental disorders, including SUDs.[113] This exclusion presently applies to Medicaid beneficiaries from ages 21-64 years and pertains to both residential and specialty M/SUD inpatient settings.[114] To expand access to care for Medicaid beneficiaries, states are now able to avoid the IMD exclusion and use Medicaid funds to pay for care in IMDs through: (1) use of Section 1115 demonstration waivers whereby states may apply to use federal funds for services in an IMD; (2) managed care rules allowing Medicaid managed care plans to pay for treatment in an IMD "in lieu of" more expensive state plan services (e.g., care in an acute general hospital setting) for no more than 15 days in a calendar month and no more than 30 days over 2 months; and (3) use of disproportionate share hospital (DSH) payments for uncompensated care costs. Very recently, state plan options under the Substance Use Disorder Prevention That Promotes Opioid Recovery and Treatment (SUPPORT) for Patients and Communities Act were authorized to enable use of Medicaid funds to cover SUD treatment in an IMD for up to 30 days in a year; this option also codifies allowance of Medicaid managed care payment in an IMD for up to 15 days in a given month.[115, 116]
This history has resulted in a patchwork of sources of state Medicaid authority to reimburse residential treatment, both in and outside IMDs, and considerable disparity between states regarding what is covered and how clear it is that residential treatment is, in any fashion, reimbursed. Some states have historically reimbursed some form of residential treatment not in an IMD (i.e., 16 or fewer beds) pursuant to their state plan,[117] and some reimburse not residential treatment per se but rehabilitation or other services provided in residential settings as well as in other locations.[118] Wyoming, for example, allows certain services to be reimbursed in residential settings, but they are treated as agency-based rather than community-based services and the setting is treated as an extension of the agency office. Thus, the services of individual or family therapy or collateral contacts are billed as agency services and regulated as they would be if the services were offered in an outpatient clinic or other setting, with the apparent result that the residential treatment facility itself is not enrolled in Medicaid.[119, 120] Some states have relied on DSH payments and/or, with changes in managed care rules, the "in lieu of" provision to cover some services provided in IMDs.[115] Increasingly, however, states are seeking Section 1115 demonstration approval from CMS to reimburse M/SUD treatment in IMDs, generally of shorter-term stays.[121]
For purposes of this Compendium, some states have no evidence of residential treatment in their Medicaid regulations or elsewhere but may allow reimbursement based on the general standards of their Medicaid program such as the "in lieu of" provision. Others have more or less detailed regulations or policy documents that address residential requirements. Finally, some have detailed Section 1115 demonstration implementation plans approved by CMS, the contents of which may or may not be reflected in regulations and/or other policy documents. Table A21 and Table A22 in the Appendix identify sources of state Medicaid authority to reimburse residential M/SUD treatment in an IMD. This Compendium and the accompanying summaries do not go into detail regarding sources of authority for treatment in nonIMDs but do include identified state requirements related thereto.
Only five states appear to have no mechanism for avoiding the IMD exclusion and covering at least some care in IMD settings. Additionally, the Medicaid reimbursement for IMD services is much more likely in a SUD than in a mental health facility. Table 16 summarizes the number of states relying on Section 1115 demonstrations, "in lieu of" reimbursement, and DSH payments for Medicaid reimbursement of M/SUD treatment in an IMD, as well as the number with no evidence of any reimbursement in an IMD. More than four times as many states have approved Section 1115 demonstrations that allow reimbursement of treatment for SUD than for mental disorder an IMD residential setting. As of early 2020, more than half of all states had approved Section 1115 waivers for SUD. The information on Section 1115 demonstrations is current as of early January 2020; however, several states have pending applications and others, doubtless, will also apply. These numbers are subject to relatively rapid change. In addition, and not included in Table 16, states such as Alaska and Oregon have Section 1115 waivers that address mental disorder residential treatment but not in an IMD.
An even larger number of states relied on the "in lieu of" provision and/or DSH payments for reimbursement of some services in an IMD. As identified in Table A21 and Table A22, many states have relied on both and some on only one these two approaches. The information about state reliance on "in lieu of" and DSH payments derives from a November 2019 synthesis by the Kaiser Family Foundation[121] that does not distinguish between payments for mental disorder versus SUD treatment or between payments for IMDs that are residential versus specialty inpatient.
Finally, the last column of Table 16 identifies that there are five states for which we found no evidence of reliance on any of the three approaches to reimbursing for treatment in any type of IMD for any M/SUD coverage. Notably, one of these five states (Idaho) presently has a pending Section 1115 application to allow coverage of residential treatment in an IMD for both mental disorder and SUD treatment.
| TABLE 16. Sources of State Medicaid Authority to Reimburse Behavioral Health Treatment in IMDs, Number of States | ||||
|---|---|---|---|---|
| Source of Authority | Mental Health | Substance Use | Mental Health and/or Substance Use |
No Evidence of Any IMD Coverage |
| 1115 demonstration (IMD residential) | 4 | 28 | ||
| "In lieu of" (residential and/or inpatient IMD)a | 33 | |||
| DSH (residential and/or inpatient IMD)a | 32 | |||
| No evidence of any IMD coverage | 5 | |||
NOTE: Detailed in Table A25 and Table A26.
|
||||
Domains Regarding Processes of Oversight
Domains regarding processes of oversight include categorization of enrollable facilities and processes of Medicaid enrollment and basic oversight.
Categorization of Medicaid facilities. As was true for licensure requirements, Medicaid enrollment requirements for residential mental health treatment are less common and less elaborate than is true for residential SUD treatment in most states. Table A23 and Table A24 include the state-by-state categorization of mental disorder and SUD residential treatment, respectively, within state Medicaid programs.
Table 17 identifies the number of states with different categorizations of residential mental disorder treatment, separated into whether the enrollment is specific to IMDs or nonIMDs. It is very common for these mental health facilities to bear unique labels that prevent categorization beyond "other." The largest number, however, are crisis facilities, some of which are specific to mental disorders and some of which also appear in the SUD table (Table 18). A total of 18 states provide evidence of Medicaid coverage for residential crisis treatment for mental disorders, four in IMDs, 15 in nonIMDs, including Massachusetts, which appears in both categories. All of these are, by definition or de facto, intended to be short-term. Among the four states where mental health services are reimbursable in a crisis facility that is an IMD, all require a statewide average length of stay of 30 days, but the District of Columbia waiver also explicitly limits the Medicaid coverage to no more than 60 days.[122] Only Texas identifies a nonIMD short-term mental disorder residential treatment facility for coverage that is not a crisis facility, although the state also covers nonIMD crisis facilities. The covered noncrisis facilities in Texas are categorized here as short-term/transitional, and they provide short-term day programs for acute needs in a residential facility with fewer than 17 beds.[123]
| TABLE 17. Number of States With Different Categories of Residential Mental Disorder Treatment Facilities That Can Enroll in Medicaid | |||
|---|---|---|---|
| IMD Status | Crisis | Short-Term/Transitional | Other |
| IMD | 4 | 0 | 0 |
| NonIMD | 15 | 1 | 16 |
| Overlap | 1 | 0 | 0 |
| * NOTE: Detailed in Table A27. Massachusetts Section 1115 waiver includes crisis units as diversionary facilities for both IMDs and nonIMDs and only for the population enrolled in managed care. Massachusetts crisis facilities are included in both rows. |
|||
Table 18 identifies the number of states with different categorizations of residential SUD treatment, separated into whether the enrollment is specific to IMDs or nonIMDs. To simplify, we relied on categories of crisis, clearly identified ASAM levels, short-term facilities, and other nonwithdrawal management and withdrawal management (WM) facilities, with overlap between categories. The large number of states with identified ASAM Level 3 or residential levels of care reflect the use of Section 1115 waivers. In addition, the IMDs that fall under either of the "other" categories reflect Section 1115 waivers where the precise levels are not identified in the waiver documents reviewed.
| TABLE 18. Number of States with Different Categories of Residential SUD Treatment Facilities That Can Enroll in Medicaid | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| IMD Status | Crisis | ASAM Level 3.1 |
ASAM Level 3.3 |
ASAM Level 3.5 |
ASAM Level 3.7 |
Short- Term |
Other NonWM |
ASAM Level 3.2-WM |
ASAM Level 3.7-WM |
Other WM |
| IMD | 1 | 21 | 17 | 21 | 18 | 25 | 5 | 15 | 16 | 5 |
| NonIMD | 7 | 8 | 5 | 7 | 5 | 5 | 11 | 3 | 4 | 6 |
| Overlap | 1 | 5 | 4 | 5 | 2 | 4 | 4 | 3 | 3 | 3 |
| NOTE: Detailed in Table A28. | ||||||||||
Processes of enrollment and basic oversight. In this section, we look at some basic indicators of oversight that may be incorporated into state Medicaid enrollment processes. Even if we were unable to determine that any residential treatment is reimbursed by a given state Medicaid program, we gathered this information to ensure that the reader is aware of the presence or absence of these processes, in the event reimbursement of residential treatment is available. Specifically, we looked at whether state licensure is required to obtain enrollment, whether duration of Medicaid is identified, whether inspection is required at enrollment or otherwise by the Medicaid agency, and whether accreditation is required for enrollment.
One of the most critical findings is that all states require that providers that wish to enroll in Medicaid be licensed or certified in accordance with applicable laws. Most states have fairly broad requirements, but some are more specific, requiring licensure for enrollment if licensure is required to provide those services in their state.[124] In theory, this leaves an opening for enrollment of provider types for which there are no licensure requirements. The general requirement of licensure or certification, however, has the very important effect of incorporating by reference all of the state licensure requirements into the Medicaid requirements, broadening state Medicaid requirements beyond what is apparent in the remainder of this section of the Compendium that focuses on explicit Medicaid requirements.
Requirements related to the duration of facility enrollment and the time between enrollment and reenrollment or revalidation are often less than precise in state Medicaid regulations. Such requirements were not located for all states and, for some, reenrollment may be required "from time to time"[125] or based on results of an audit (e.g., Vermont, every 1-3 years).[126] It is important to note, however, that this requirement, as well as others such as inspections by the Medicaid agency or accreditation requirements imposed by the Medicaid agency, may be reflected in other documents rather than in regulations. Locations for requirements related to enrollment also might include provider agreements with Medicaid or MCEs, provider manuals, or enrollment guidance on state websites. Similarly, some states may rely on licensure requirements to ensure that inspections occur or, in some cases, that accreditation is required.
| TABLE 19. Number of States with Different Processes of Medicaid Enrollment Fully or Partially Present | ||
|---|---|---|
| Requirements | Mental Health | Substance Use |
| State licensure/certification required | 51 | 51 |
| Enrollment duration specified | 13 | 15 |
| Inspections by Medicaid agency required | 11 | 10 |
| Accreditation required | 3 | 4 |
| NOTE: Detailed in Table A29. | ||
Domains Regarding Facility Operations
Domains regarding facility operations include standards regarding staffing, placement, treatment and discharge planning, care coordination and aftercare requirements, treatment services provided (including MAT), quality assurance or improvement, and requirements related to special populations.
Staffing standards. Qualified staff at all levels are important to the provision of quality care in residential treatment. In our examination of state Medicaid requirements, we examined, first, requirements regarding staffing (Table 20) and, second, regarding staff training (Table 21).
The focus of the first was on quantifiable standards, such as whether there are any requirements related to facility administrators, medical directors, other medical staff, clinical staff, or direct care staff. States may approach this as simply as requiring that there be an administrator, or, instead, may specify educational credentials and/or experience. We also examined the extent to which states incorporate staffing ratios and/or require that there be "sufficient" or "adequate" staffing. Finally, in order to provide an overall sense of whether the Medicaid standards reviewed included any staffing requirements, Table 20 also provides that information. As may be seen in Table 20, specific staffing requirements as part of state Medicaid regulations are relatively uncommon but more frequently found, for some or all Medicaid-enrolled facilities, regarding SUD than mental disorder residential treatment.
As noted before, however, all state Medicaid programs require appropriate licensure or certification of enrolled providers (both facilities and individual providers), and it appears that most rely on the licensure requirements for explicit staffing standards related to specific facility types. Similarly, many state Medicaid programs no doubt rely on M/SUD provider manuals or on contracts between the Medicaid agency or its MCEs and providers. In addition, states with Section 1115 waivers are required to implement certain activities related to staffing, with waiver documents usually including requirements that the state "establish residential treatment provider qualifications in licensure, policy or provider manuals, managed care contracts or credentialing, or other requirements or guidance that meet program standards in the ASAM Criteria or other nationally recognized, SUD-specific program standards regarding credentials of staff for residential treatment settings."[127] As an example, Michigan has implemented requirements in its provider manual[128] and requires by contract that its Medicaid health plans "conduct ongoing validation and revalidation of provider credentials."[127] More significantly, both those waivers and separate requirements put in place by states lead to incorporation of the ASAM standards as expectations for facilities providing SUD residential treatment. The ASAM standards vary in the degree to which they specify staffing type, but the Level 3.7-WM standards in particular are fairly detailed regarding medical personnel.[28]
| TABLE 20. Number of States with Medicaid Requirements for Staffing in Residential Facilities | ||
|---|---|---|
| Requirements | Mental Healtha | Substance Usea |
| Standards | ||
| Administrator | 4 | 5 |
| Medical director | 1 | 3 |
| Medical staff | 8 | 16 |
| Clinical staff | 8 | 15 |
| Direct care staff | 5 | 8 |
| Staffing levels | ||
| Include ratios | 3 | 3 |
| Require adequate staffing | 5 | 4 |
| Any staffing requirements | 24 | 35 |
NOTE: Detailed in Table A30.
|
||
For the second aspect of staffing, we looked at: (1) orientation and ongoing training requirements; (2) two selected potential foci of training, specifically staff training regarding trauma-informed care and regarding suicide assessment and/or prevention (or crisis training); and (3) whether any Medicaid requirements existed regarding staff training. Very few states include requirements regarding staff training in Medicaid regulations for some or all Medicaid-enrolled facilities (Table 21), although it is possible that more exists in the form of contracts with providers. With regard to our two exemplar training topics, trauma-informed care and suicide assessment/prevention or crisis training, only one state Medicaid program required training related to either in the documents examined or pursuant to state staff report. Nebraska Medicaid requires, for psychiatric residential rehabilitation, that all staff be educated or trained in trauma-informed care,[118] and Maryland Medicaid requires, for all Level 3 SUD treatment facilities, that there be staff trained in crisis intervention or management.[129]
| TABLE 21. Number of States with Medicaid Requirements for Staff Training in Residential Facilities | ||
|---|---|---|
| Requirements | Mental Healtha | Substance Usea |
| Orientation and/or ongoing training |
1 |
2 |
| Trauma-informed care training |
1 |
0 |
| Suicide assessment/prevention or crisis training |
0 |
1 |
| Any training requirements |
4 |
6 |
NOTE: Detailed in Table A31.
|
||
Placement standards. Placement in the appropriate setting and level of care is important to ensure that patients receive the care they need and that Medicaid funds are not expended for either unnecessary or inadequate care. To determine whether state Medicaid agency placement oversight exists, we examined whether there were specific criteria for placement and/or assessment, for some or all Medicaid-enrolled facilities, including whether regulations delegated this by way of facility policy and procedure requirements. Within the realm of SUD treatment, we looked at Medicaid requirements related to use of the ASAM Patient Placement Criteria. We exclude from the numbers shown in Table 22 basic requirements for prior authorization, which act as a filter for payers such as Medicaid. Many of the detailed state summaries, however, mention requirements for prior authorization as well as requirements for continued stay and discharge criteria.
As Table 22 indicates, specific placement criteria were identified in Medicaid requirements in slightly less than half and nearly four-fifths of the states for mental disorder and SUD residential treatment respectively. Somewhat fewer of each included language clearly providing information regarding the process of placement assessment or screening. The larger number for SUD treatment reflects, in large part, adoption of the ASAM placement criteria, identified as necessary in 31 of 51 jurisdictions, many through standard Section 1115 IMD waiver requirements as well as waiver implementation plans. Nearly universal language for the approved demonstrations specifies that the state must establish a requirement that providers and sometimes MCEs "assess treatment needs based on SUD-specific, multidimensional assessment tools, such as the ASAM Criteria or other comparable assessment and placement tools that reflect evidence-based clinical treatment guidelines." The state also is required to establish "a utilization management approach such that beneficiaries have access to SUD services at the appropriate level of care and that the interventions are appropriate for the diagnosis and level of care, including an independent process for reviewing placement in residential treatment settings."[130] Unlike state licensing requirements, state Medicaid programs do not typically have a practice of requiring facilities to adopt policies and procedures to address placement. Rather, it is likely that states rely on the fact that licensure requirements often take that approach. It also is possible that Medicaid programs have these and other requirements in provider agreements with Medicaid or MCEs or in provider manuals.
Of separate interest are the requirements that are found for residential mental disorder treatment. Most requirements involve descriptions of whom different types of residential treatment are designed to serve. Some specify that assessments occur to ensure that placement is correct. There are, however, at least three states with somewhat specific requirements related to identified tools for placement. All three have different approaches to these requirements. The District of Columbia has an approved Section 1115 waiver permitting Medicaid coverage for both mental disorder and SUD residential treatment. The approval required adoption of "an evidence-based, publicly available patient assessment tool, preferably endorsed by a mental health provider association (e.g., LOCUS or CASII) to determine appropriate level of care and length of stay," and the District has opted to use the "Level of Care Utilization System (LOCUS) level of care assessment tool to ensure that services to adults are individualized, clinically appropriate, and least restrictive. The LOCUS assists in determining the appropriate level of care and treatment interventions are based on individualized clinical assessments. LOCUS evaluations must be used at intake, during treatment plan development, when a consumer is in crisis, and when a level of care change is needed."[122] In contrast, Nevada has adopted the LOCUS as part of the state Medicaid Services Manual,[131] which is incorporated by reference into the administrative rules, and Maine agency staff indicated during validation that the LOCUS is required by the state Medicaid program.[132]
| TABLE 22. Number of States with Medicaid Requirements for Placement in Residential Facilities | ||
|---|---|---|
| Requirements | Mental Healtha | Substance Usea |
| Specific placement criteria identified | 22 | 38 |
| Placement assessment/screening | 14 | 33 |
| ASAM for placement | 0 | 31 |
| Policies or procedures | 0 | 0 |
NOTE: Detailed in Table A32.
|
||
Treatment and discharge planning, care coordination, and aftercare requirements. Solid treatment and discharge planning are critical to ensuring appropriate treatment that is focused on recovery and next steps as well as on immediate needs. Care coordination and aftercare relate to planning for the present and the future.
Approximately one-third to one-half of state Medicaid programs have explicit requirements for treatment planning, for some or all Medicaid-enrolled facilities (Table 23). Fewer incorporate requirements for discharge planning, and very few Medicaid programs are explicit that discharge planning should begin at or near admission (mental health: three; substance use: five). Few Medicaid programs incorporate express requirements for follow-up with discharged clients or the continued provision of aftercare by the residential facility. Those that do include Vermont, which requires follow-up with both the patient and receiving provider within 72 hours after discharge from mental disorder residential treatment;[126] New Hampshire, which requires "active outreach" to clients following discharge;[133] and New Mexico, which requires follow-up after discharge from crisis stabilization services.[134]
The relative paucity of some of these standards in state Medicaid regulations does not mean that the programs do not have such requirements, because they may be in provider agreements with Medicaid or MCEs or in provider manuals. Similarly, some states may rely on the presence of licensure requirements to ensure that treatment and discharge planning requirements, in particular, apply to facilities. Additionally, those programs that incorporate the ASAM standards also effectively incorporate the ASAM principle that an individualized assessment-based treatment plan should be developed.[28]
As states seek to integrate all aspects of physical and M/SUD care, care coordination has received greater emphasis. Care coordination requirements were located in more than one-third of state Medicaid mental health requirements and nearly four-fifths of state Medicaid SUD requirements. The number of states with SUD treatment care coordination requirements reflects, in part, the nearly universal requirement in Section 1115 waivers allowing reimbursement of SUD treatment in IMDs that "beneficiaries will have improved care coordination" and requiring the state to ensure the establishment and implementation of policies to ensure residential facilities "link beneficiaries with community-based services and supports, including tribal services and supports, following stays in these facilities within 24 months of SUD program demonstration approval."[135] States use different approaches to meet this mandate. Washington State, for instance, relies heavily on its MCEs and as part of waiver implementation is implementing a requirement that "MCOs [managed care organizations], residential treatment providers, and outpatient providers work to develop policies and practices that enhance care coordination, including transitions between levels of care following residential treatment stays."[135] Oklahoma, which does not have a Section 1115 waiver, has in place a program of Behavioral Health Case Management available to individuals transitioning from nonIMD institutions to the community. "Individuals are considered to be transitioning to the community during the last thirty (30) consecutive days of a covered institutional stay. This time is to distinguish case management services that are not within the scope of the institution's discharge planning activities from case management required for transitioning individuals with complex, chronic, medical needs to the community. Transition services provided while the individual is in the institution are to be claimed as delivered on the day of discharge from the institution."[136]
| TABLE 23. Number of States with Medicaid Requirements for Treatment and Discharge Planning, Care Coordination, and Aftercare in Residential Treatment | ||
|---|---|---|
| Requirements | Mental Healtha | Substance Usea |
| Treatment plan required | 18 | 26 |
| Discharge plan required | 8 | 17 |
| Discharge plan early | 3 | 5 |
| Care coordination | 20 | 37 |
| Aftercare/follow-up | 1 | 2 |
NOTE: Detailed in Table A33.
|
||
Treatment services. Ensuring the use of evidence-based or best practice treatment is crucial to providing high-quality M/SUD residential services. Given the range of types and levels of treatment, we focused on whether therapeutic services were required by the regulations, if amount was specified, and whether states included requirements regarding evidence-based or best practice treatment. One specific evidence-based practice, examined within the realm of service delivery, was medication treatment as part of MAT specific to residential settings, which is discussed in greater detail below.
All Medicaid programs require medical necessity for services in order to obtain reimbursement. More detailed Medicaid service requirements for some or all Medicaid-enrolled facilities, however, are found most often regarding residential SUD treatment in contrast to residential mental disorder treatment (Table 24). The increasing adoption by states of the ASAM standards, whether as part of a Section 1115 waiver mandate to establish "residential treatment provider qualifications in licensure, policy or provider manuals, managed care contracts or credentialing, or other requirements or guidance that meet program standards in the ASAM Criteria or other comparable, nationally recognized, SUD-specific program standards regarding in particular the types of services, [and] hours of clinical care, ... for residential treatment settings,"[137] or otherwise, contributes to this distinction. Some states, however, have taken additional steps. Ohio, for example, provides that "individuals in residential treatment may receive medically necessary services from practitioners who are not affiliated with the residential treatment program. Examples include, but are not limited to, psychiatry, MAT, or other medical treatment that is outside the scope of the residential level of care as defined by ASAM. Medicaid reimburses providers of these services outside the per diem rate paid to residential treatment programs."[138]
As also may be seen in Table 24, only five states were found to have explicit regulatory or waiver-based Medicaid requirement regarding use of evidence-based practices for mental disorder residential treatment. Michigan and Nevada, for instance, require that evidence-based practices be used for both mental disorder and SUD residential treatment.[128, 131] In contrast, 31 states require use of evidence-based practices in some aspects of Medicaid-reimbursed residential SUD treatment, many by requiring access to MAT (see also Table 25), but some are specific about other evidence-based practices. For example, the Maryland Medicaid regulations require participating adult residential treatment facilities to demonstrate competence in the ability to deliver a minimum of three evidence-based practice services.[139]
| TABLE 24. Number of States with Medicaid Requirements for Services in Residential Facilities | ||
|---|---|---|
| Requirements | Mental Healtha | Substance Usea |
| Any service requirements | 20 | 38 |
| Specific to clinical service types | 17 | 38 |
| Specific to clinical service hours | 2 | 28 |
| Evidence-based | 5 | 31 |
NOTE: Detailed in Table A34.
|
||
Review of state Medicaid requirements revealed that 31 of 51 jurisdictions explicitly call for the provision of MAT in residential SUD treatment settings or that access to an outside provider be a component of treatment in the residential facility, for some or all Medicaid-enrolled facilities (Table 25). Most Section 1115 waivers permitting reimbursement of SUD treatment provided in residential IMD facilities include requirements that the state: (1) undertake "an assessment of the availability of providers in the key levels of care throughout the state, or in the regions of the state participating under this demonstration, including those that offer MAT"; and (2) establish a requirement that residential treatment providers offer MAT on-site or facilitate access to MAT off-site."[126] States implement this along different timeframes, but Vermont, for example, already required that MAT be offered in all residential programs.[126] Two states with Section 1115 waivers that permit residential treatment in an IMD, Maryland and Massachusetts, reimburse MAT, but their waiver documents do not incorporate it into residential settings.[140, 141]
| TABLE 25. Number of States with Medicaid Requirements for MAT in Residential Facilities | ||
|---|---|---|
| Requirements | Mental Healtha | Substance Usea |
| MAT required | 0 | 31 |
NOTE: Detailed in Table A35.
|
||
Quality assurance or improvement. Explicit requirements for quality assurance or improvement programs imposed directly on facilities were relatively rare in the Medicaid regulations or in Section 1115 waiver documents, for some or all Medicaid-enrolled facilities (mental health: nine; substance use: ten) (Table 26). Requirements for measurement or data submission (beyond claims or encounters data) (mental health: two, substance use: five) were even less common. This, however, does not mean that Medicaid programs may not have such requirements because they may appear in provider agreements with Medicaid or MCEs, in provider manuals, or on state websites. Similarly, some states may rely on the presence of licensure requirements to ensure that quality assurance or improvement requirements apply to facilities.
It also is important to note that state contracts with MCEs impose QA/QI requirements on the MCE, which MCEs may or may not translate into requirements imposed on their network providers. Additionally, Section 1115 demonstrations nearly always include requirements designed to ensure quality of services that apply to the state itself as manager of the demonstration. In the Section 1115 waivers that allow reimbursement for SUD services in an IMD, there is a nearly uniform requirement similar to that found in the North Carolina approval that the state must establish "a provider review process to ensure that residential treatment providers deliver care consistent with the specifications in the ASAM Criteria or other nationally recognized SUD program standards based on evidence-based clinical treatment guidelines for types of services, hours of clinical care, and credentials of staff for residential treatment settings within 12-24 months of SUD program demonstration approval."[142] States then address implementation in different ways in their individual SUD implementation plans, for example, by assuring CMS that licensing requirements do or will reflect ASAM criteria or by promising expanded facility monitoring.[142] Requirements such as these related to licensing requirements reflecting ASAM criteria or monitoring, however, are not the same as requiring that residential facilities themselves develop and undertake an explicit QA/QI program.
| TABLE 26. Number of States with Medicaid Requirements for QA/AI | ||
|---|---|---|
| Requirements | Mental Healtha | Substance Usea |
| QA/QI required | 9 | 10 |
| Measurement/data | 2 | 5 |
NOTE: Detailed in Table A36.
|
||
Special populations. State Medicaid requirements regarding residential M/SUD treatment pertinent to special populations are rare, for some or all Medicaid-enrolled facilities and, when seen, generally relate to treatment of co-occurring M/SUD conditions or treatment of pregnant women (Table 27). In the miscellaneous category of "other" special populations, regulations found included references to a number of disparate groups, such as those with co-occurring mental and physical health conditions[126] or "adults with I/DD and severe psychiatric or behavioral symptoms following a crisis event and/or psychiatric inpatient stay and/or transitioning out of the criminal justice system or a long-term (2 or more years) institutional placement (including residential psychiatric treatment facility)."[143]
More commonly, state Medicaid programs or other state agencies that have adopted the ASAM criteria for SUD treatment are essentially incorporating the ASAM standards for those with co-occurring mental disorders.[28] Similarly, it is increasingly common to find states that are subject to explicit requirements in Section 1115 waivers regarding, in particular, treatment of co-occurring disorders. Nearly all Section 1115 approved waivers that permit Medicaid reimbursement of SUD treatment in IMDs require that the waiver be used to improve "care for co-morbid physical and mental health conditions."[134] The implementation of this is reflected in different ways. For example, in its submitted SUD implementation plan, New Mexico plans to include ASAM levels "3.2, 3.3, and 3.5 in adult accredited residential settings for individuals with SUD and co-occurring conditions."[134]
| TABLE 27. Number of States with Medicaid Requirements Related to Special Populations | ||
|---|---|---|
| Requirements | Mental Healtha | Substance Usea |
| Co-occurring M/SUDs | 6 | 29 |
| Pregnant/parenting women | 2 | 8 |
| Other | 4 | 2 |
NOTE: Detailed in Table A37.
|
||
SECTION 4. DISCUSSION AND SYNTHESIS
The primary purpose of this Compendium and its accompanying state summaries is to develop a better understanding of the landscape of state regulation and oversight of M/SUD residential treatment. One of the first tasks was to decide what constituted M/SUD residential treatment. Doing so made it clear that, aside from the Level 3 facility standards found in the ASAM criteria, there are no consistent and common definitions. To define and bound the scope of this research, we took the approaches, discussed in our methodology, of requiring clinical treatment in the residential settings and of excluding certain categories of facilities. Even after using this approach, this study makes evident that there are many labels for residential treatment in the United States, as well as residential settings that are not included in this research. Despite this limitation, the study framework, with primary domains of oversight and operations, allowed us to look at the landscape of incorporated facilities methodically.
Oversight
Bifurcated and trifurcated systems. As is true of other forms of M/SUD treatment, and despite ongoing efforts to integrate care in the United States, mental disorder and SUD treatment in residential settings often remains bifurcated, in terms of: (1) who is being treated in different facilities; (2) who is overseeing many of those facilities; and (3) how extensive the range of comparative oversight is for the two broad categories of M/SUD residential treatment. The addition of separate Medicaid agencies further divides oversight and regulation.
-
Distinctions commonly remain as to whether a given type of facility is intended to treat mental disorders versus SUDs. This most often hinges on whether facilities are distinctly created for one or the other, in contrast to being, for instance, crisis facilities designed to treat both.[144] Refinements exist, such as permitting treatment for SUD in a mental health residential facility if a person's primary diagnosis falls into the mental disorder category. In addition to crisis facilities designed for both, however, this distinction is increasingly breaking down in the realm of SUD treatment, in which it is widely acknowledged that many individuals with SUD also have a mental disorder and that they must be treated concurrently. This need for concurrent treatment is recognized in an increasing number of states that specifically call by statute or regulation for treatment of co-occurring conditions[145] and in the ASAM criteria,[28] which are increasingly adopted by states to structure and define their SUD treatment. Many states, however, have not taken such steps and, ones that do, tend to approach it from the SUD side of behavioral health.
-
This phenomenon relates to the often bifurcated nature of state oversight, with separate agencies or, at least, separate subagencies still common regarding licensure and/or other oversight. States are increasingly opting to combine all behavioral health into one agency. Even when this combination occurs, however, internal silos may remain that still must be breached in order to fully coordinate oversight of all behavioral health in a given state.
-
As was evident from the findings in the separate sections of this Compendium dealing with state: (1) licensure and related standards; and (2) Medicaid regulation of M/SUD residential treatment, there is considerable disparity in the extent to which states regulate mental disorder versus SUD residential treatment. SUD residential treatment presently has far greater structure and oversight in many states. The likely reasons for this are three-fold.
-
The opioid epidemic has forced state legislatures and agencies in recent years to give particular attention to expanding and overseeing SUD treatment. This is partly reflected in state regulations and policies.
-
In recent years, parity legislation and Medicaid expansion have combined with the opioid epidemic to increase avenues for reimbursement of treatment for SUD more rapidly than parity and Medicaid expansion alone might have, leading to greater attention to facilitating access to and reimbursement of SUD treatment compared with mental health treatment. Thus, we see burgeoning opportunities and new avenues for financing SUD treatment, including within IMDs. SAMHSA's Projections of National Expenditures for Treatment of Mental and Substance Use Disorders, 2010-2020[146] predicted increased spending for SUD relative to mental disorder treatment. In addition, supplemental government spending, such as that resulting from the SUPPORT Act and funds provided through the SAMHSA State Targeted Response and State Opioid Response grants, resulted in substantial funding available to address the opioid epidemic.
-
The increased funding that came with changes regarding IMDs has also brought changes in requirements accompanying the funding. We also see an even larger patchwork of oversight and opportunity. The incorporation of ASAM placement, treatment, staffing, and other requirements has influenced far more than treatment in IMDs. As states may increasingly seek Section 1115 waivers for treatment in IMDs of individuals with SMI as well as SUD, comparable attention to regulation and oversight of mental disorder residential treatment may follow suit.
-
Unregulated facilities. Our examination of state regulations and statutes, state Medicaid requirements, and, to a limited extent, policy documents, indicates that there are intermittent gaps or potential gaps in regulation and licensure of residential treatment facilities. Figure 3 presents an overall picture of the extent to which oversight generally does or does not exist in the states on the basis of the data sources used for this study. For residential mental disorder and SUD treatment facilities, we provide counts, based on the documentation examined for this study, of: (1) the number of states in which all residential treatment facilities are regulated and/or licensed; (2) the number of states where some are regulated and/or licensed; (3) the number with evidence of ability to enroll in Medicaid; and (4) the total number that meet at least one of those criteria.
From these data, we see that all states but four have some form of oversight of residential mental disorder treatment and all 51 states do so for residential SUD treatment, either through state licensure and oversight standards, applicable state Medicaid requirements, or both. Additional detail is available in the detailed tables at Appendix A, but the four states with no apparent regulatory oversight specific to residential mental disorder treatment facilities are Idaho, New Jersey, North Dakota, and South Dakota. It is important to realize, however, that these states may oversee and mandate standards via contracts with providers. Additionally, as is true for New Jersey, states may have an array of regulated mental health residential facilities (e.g., residential health care facilities, supervised residences for adults with mental illness) that do not require treatment as a component of services.
Processes of regulation, oversight, and licensure. Facilities in some states may be subject to multiple sets of state oversight, licensure, or certification and, on occasion, state licensure standards also may require accreditation or provide "deemed status" for optional accreditation. Accreditation by an independent accrediting body such as TJC, the Commission on Accreditation for Rehabilitative Facilities, or the COA can provide yet another layer of oversight and inspection, beyond that carried out by the states. When accreditation takes the place of oversight, however, it is imperative--and many states are clear on this point--that the accreditation standards must cover and address the state standards that will not be a focus of oversight by the state. States typically retain authority, even in the event of deemed status, to conduct cause-based investigations and inspections. Indeed, provision for state inspection is an important indicator of opportunities for concerted oversight.
Analysis of inspection requirements found that most states have some provision for inspections of some or all M/SUD residential treatment facilities. On the basis of the information in state summaries, we looked at whether there were any inspection requirements associated with licensure, at any point and for any reason, and at whether there were any inspection requirements associated with Medicaid enrollment, at any point and for any reason.
As shown in Figure 4, out of 51 jurisdictions, 48 had provisions for inspection at licensure, post-licensure, or some point in Medicaid enrollment for mental disorder residential treatment and 50 had provisions for inspections of SUD residential treatment. Most of the four states without any apparent provision for inspection for mental health facilities, did not have any identified regulated mental health residential facilities.
| FIGURE 4. Number of States with Inspections of Residential Treatment Facilities |
|---|
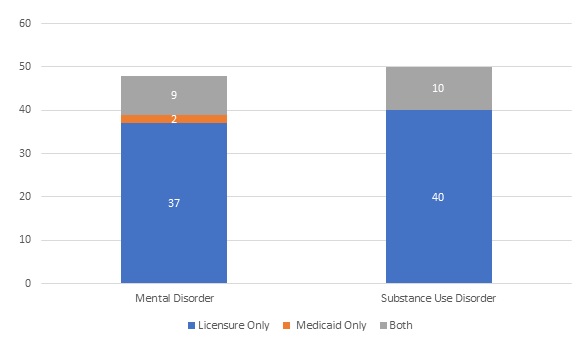 |
Intersection of licensure and Medicaid in the imposition of standards. All states require that providers that wish to enroll in Medicaid be licensed or certified in accordance with applicable laws, assuming applicable laws exist in the state. This requirement pertains equally to facility providers, such as residential treatment programs, and to individual providers. This requirement has the very important effect of incorporating by reference all state licensure requirements into the Medicaid requirements, broadening state Medicaid requirements beyond what is explicit in Medicaid regulations, waivers, or other documents. Because Medicaid is the largest payer for behavioral health services in the United States, these requirements have broad effect on a large population. Especially for SUD treatment, the spate of new state regulatory requirements and of approved Medicaid waivers, the latter of which can influence state regulatory requirements, there may be a synergistic effect.
Operations
Access and placement. Access to and placement in treatment are related. Access to residential treatment is most often addressed in regulations as functions of nondiscrimination and of physical access. This study examined access in the context of wait times and, although states occasionally address wait times in regulations, it is more commonly a feature of other policy documents, state website portals, or contractual requirements. The latter can include requirements imposed on Medicaid MCEs regarding network adequacy. Additionally, within the context of residential treatment where time is often of the essence and placements are scarce, formal measured wait times may be less meaningful than for outpatient treatment in the community. Especially if Medicaid does not reimburse for residential M/SUD treatment, what is most likely to happen may be settling for a second-best level of care, whether inpatient, intensive outpatient, or other outpatient treatment. This relates, therefore, to appropriate placement because absent access, placement may not be ideal.
| FIGURE 5. Number of States with Provisions for Placement Criteria Specific to Residential Treatment |
|---|
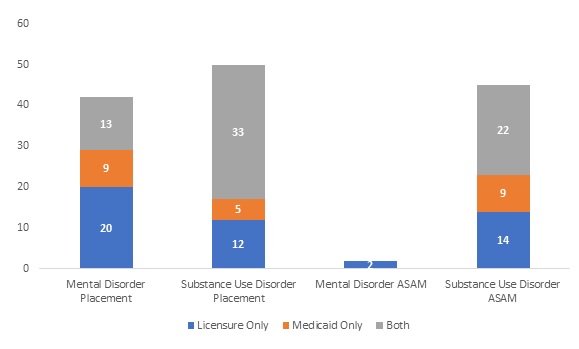 |
Specific placement criteria for residential treatment facilities are the norm, derived from a combination of licensure-related and Medicaid requirements; 42 and 50 states were found to include such requirements for mental disorder and SUD residential treatment, respectively (Figure 5). As might be expected, required use of the ASAM Patient Placement Criteria were nearly exclusively limited to residential SUD treatment. A total of 45 states specifically use the ASAM criteria for placement in SUD treatment, and many of those states include those with Section 1115 IMD demonstrations. Two states, Indiana and Utah, also require that it be used in mental disorder residential treatment when appropriate.[75, 147] Many states also have, in addition to standards of placement, criteria for continued stay and/or discharge. These appear both in licensure-related standards and in Medicaid requirements. We did not see any single set of placement criteria predominant through the mental health residential requirements. The best-known placement approach, the LOCUS, was mentioned no more than once or twice in the regulatory review. We are aware, however, from our interviews with experts that more states are using it and requiring its use via contract and other mechanisms. It is possible that its use will increase as more states receive approval of Section 1115 demonstrations related to the provision of services to individuals with SMI.
Treatment and discharge planning. States are more likely to include treatment planning and discharge planning requirements in licensure and other nonMedicaid standards than they are as Medicaid requirements, although a number do that as well (Figure 6). Documentation examined revealed that treatment planning requirements were included for 46 and 50 states, respectively, for mental disorder and SUD residential treatment. Somewhat fewer included discharge planning requirements, 40 and 49 states for mental disorder and SUD residential treatment, respectively. These high levels indicate a concern that treatment be appropriately planned and that provision for ongoing treatment and support after discharge should be an essential component of services, preferably beginning early in the treatment process.
| FIGURE 6. Number of States with Provisions for Treatment and Discharge Planning Specific to Residential Treatment |
|---|
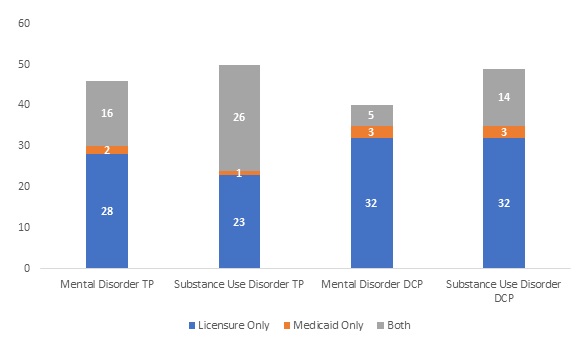 |
Requirements related to aftercare services or follow-up. State standards for, if not requirements for the provision of, aftercare services or follow-up after discharge from a residential facility are rare, particularly on the Medicaid side in regulations and waivers. As a reminder, in discussing aftercare services and follow-up requirements, we are not discussing discharge planning and referrals but, rather, practices in which the residential facility discharging the individual continues some ongoing service or follows up on the status of the individual post-discharge. When such provisions exist, they are designed to either: (1) provide a bridge for services until the person is established in a new setting; or (2) allow the discharging facility to know whether referred post-discharge services are being accessed and if they are successful. As Figure 7 displays, six and 13 states include such requirements for mental disorder and SUD residential treatment, respectively, primarily in licensure or other nonMedicaid standards. Interestingly, there is no overlap between licensure and Medicaid requirements, and only one state includes aftercare or follow-up provisions for both sides of M/SUD residential treatment--that is follow-up after crisis services.[148]
The three state Medicaid programs in which such requirements were located all focused on required follow-up after discharge from mental disorder residential treatment (Vermont),[126] from SUD residential treatment (New Hampshire),[133] or from SUD crisis stabilization services (New Mexico).[134] Similarly, requirements in ten states, including for mental disorder residential treatment--Illinois, Iowa, Kansas, Oklahoma, and Washington, and for SUD residential treatment--Iowa, Massachusetts, Ohio, Oklahoma, Oregon, and Wisconsin--involved follow-up and not ongoing treatment by the residential facility.[149] In contrast, Wyoming requires, for detoxification facilities, provision for referral, escort, and transportation to other treatment services, as necessary, to ensure that continuity of care is provided.[150] Michigan,[151] Pennsylvania,[152] and South Carolina[153] apparently envision both follow-up and potential provision of aftercare services by at least some of their licensed SUD residential treatment facilities. Hopefully, these relatively few standards related to ensuring follow-up and the provision of aftercare as a bridge service indicate a trend that will evolve further. As we seek to improve retention in treatment, ensuring follow-on care after residential placement is important.
| FIGURE 7. Number of States with Provisions for Aftercare Specific to Residential Treatment |
|---|
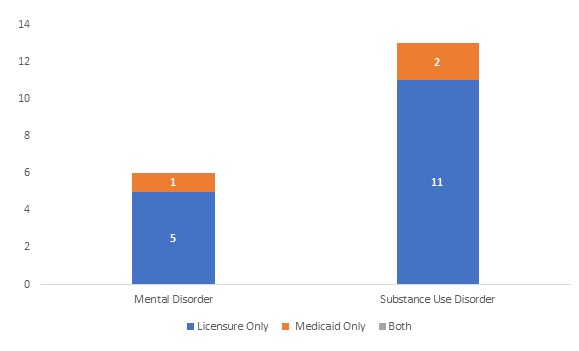 |
Standards for treatment services. In addition to assessments related to placement, treatment planning, and coordination of care, treatment services in the form of psychosocial and medication treatment are key components of residential treatment. The states vary in the extent to which they elaborate, some being very specific and others less so. In the SUD treatment realm, however, Level 3 standards increasingly are being adopted, with different degrees of fidelity and specificity, from the ASAM criteria, driven in part by Section 1115 Medicaid demonstration requirements. Two discrete indicators of states wading into the prescribing of services are the extent to which: (1) evidence-based practices; and (2) MAT are overtly required regarding residential treatment.
-
Evidence-based care can be difficult to define. For this study, we looked at whether states had explicit requirements for "evidence-based" practices or "best practices." We also included states where either trauma-informed care, motivational interviewing, or MAT is explicitly required to be used or, in the case of the latter, available, although these requirements may vary by facility type within states. We recognize that there are other evidence-based practices, but these are the ones that are most likely to be clearly included as requirements. SUD residential treatment facilities are most likely to have requirements for evidence-based practices, with 43 out of 51 states including some form of requirement (Figure 8), most commonly MAT. In contrast, only 16 states, in total, incorporated requirements specific to evidence-based practices for residential mental disorder treatment. This difference between mental disorder and SUD treatment might seem unwarranted, but many of the requirements related to MAT are waiver-driven Medicaid requirements that also appear to be seeping into SUD licensure and other nonMedicaid oversight standards. This suggests that wider use of Section 1115 waivers for mental health services might have similar effect.
| FIGURE 8. Number of States with Requirements for Evidence-Based Treatments Specific to Residential Treatment |
|---|
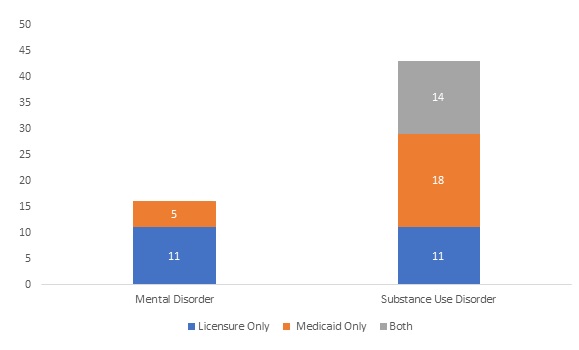 |
-
Figure 9 displays the number of states that have any requirements in place specific to residential treatment regarding access to MAT. As would be expected, they are much more commonly specific to SUD treatment facilities, with a total of 39 states having SUD licensure-related and/or Medicaid-related requirements in place. These numbers, however, may include some states that address MAT only for a subset of regulated residential facilities (e.g., publicly-funded), and, likewise, Medicaid requirements apply only to Medicaid-enrolled providers and, in some cases, perhaps only to IMDs or nonIMDs. However, a significant portion of the Medicaid requirements reflect the existence of Section 1115 waivers, the number of which presumably will continue to increase. Additionally, the inclusion of requirements related to MAT in residential treatment, even if only directly applicable to certain facilities or certain populations depending on funding or other factors, means that it is more likely that other facilities and individuals in the state will experience spillover as MAT becomes more widely available. Additionally, the Section 1115 demonstrations are laboratories for innovation that may spread best practices to other states.
Of separate interest, however, are the two states, Maryland and Utah, that also have licensure or other oversight requirements regarding MAT that apply equally to residential mental disorder and SUD treatment facilities. In Maryland, no Behavioral Health Authority-licensed community-based M/SUD programs may exclude or discriminate against an individual on the basis of the individual receiving opioid treatment services.[91] In Utah, all service providers contracting with the Division of Substance Abuse and Mental Health and all County Local Authority programs must provide written information to every treatment participant regarding rights to MAT[93] and, in community-based treatment programs, all individuals with AUDs and/or OUDs must be educated and screened for the potential use of MAT.[94] Although neither of these requirements go so far as to require access to MAT in a residential mental disorder treatment setting, they do pave the way for better care integration and access to MAT for all individuals needing residential care regardless of primary diagnosis.
| FIGURE 9. Number of States with Provisions for MAT Specific to Residential Treatment |
|---|
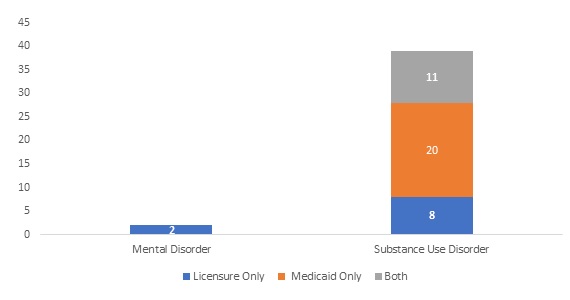 |
Staffing requirements. Staffing standards may include requirements regarding hiring, credentialing, training, documentation of employment requirements or practices, and staffing levels, among other things. This is one area where policy documents and contracts may be better suited for states to set standards, allowing greater flexibility than is possible with regulations or statutes, particularly with the many different types of treatment and evolving service needs involved in behavioral health treatment.
As one indicator of state involvement in staffing standard-setting, we looked at staffing levels. Adequate staffing levels are needed to ensure quality treatment and safety in 24-hour M/SUD settings. Figure 10 illustrates the status of staffing level requirements specific to residential treatment in the 51 states. A total of 39 states had staffing ratios and/or requirements for adequate or sufficient staffing in mental disorder residential treatment facilities. Forty-four states did for SUD residential treatment. Most such requirements sprang from licensure and other nonMedicaid standards and were, predominantly, not ratios.
| FIGURE 10. Number of States with Provisions for Staffing Levels Specific to Residential Treatment |
|---|
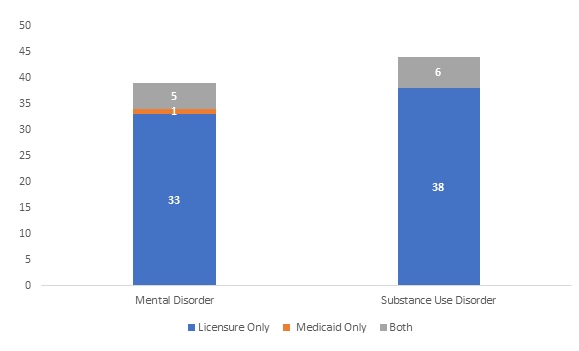 |
Quality assurance/quality improvement requirements. The scope and nature of QA/QI requirements applicable to residential M/SUD treatment vary considerably and not all apply equally to all facility types. It is possible, however, to say that some form of explicit requirement imposed on the facility is common. As Figure 11 shows, this is truer for SUD than mental disorder treatment and generally stems from licensure and related oversight standards rather than from state Medicaid requirements. In the documentation examined, we identified 38 and 48 states that impose some such requirement for residential mental disorder and SUD treatment facilities, respectively. Of note, however, some states incorporate such requirements into contracts with providers or other policy documents and, in the realm of Medicaid requirements, also may incorporate such requirements into contracts between the state and the MCE. In the latter case, the requirements on the MCE may be strictly on the MCE or may include requirements to impose specific QA/QI responsibilities on their network of providers. In any event, it is promising to see the extent to which some type of QA/QI requirement is a part of state expectations for residential treatment. Because what is perceived as quality may change over time, however, the rigid regulations may not be best to elaborate in detail on what is required.
| FIGURE 11. Number of States with Provisions for QA/QI Specific to Residential Treatment |
|---|
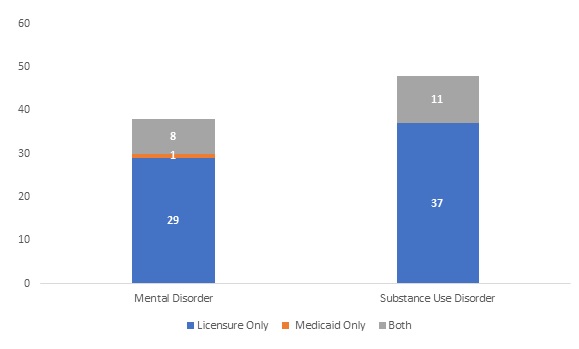 |
Service recipient rights and governance. We examined service recipient rights and governance standards only with regard to requirements not specific to Medicaid. Both are much more commonly reflected in state nonMedicaid-related requirements than in Medicaid requirements.
-
Statutes and regulations governing service recipient rights evolved out of a history of maltreatment in some institutions. We looked at two discrete aspects of service recipient rights, related to: (1) the right to voice grievances, taken as an indicator of the ability of service recipients to enforce their rights in general; and (2) rights related to restraint and seclusion, because restraint and seclusion affect both safety and dignity. The first, the right to voice grievances, is more commonly provided for in regulations than is the second, rights regarding restraint or seclusion.
-
Governance standards are elaborate in some states and nonexistent in others, with regard to residential M/SUD treatment. These standards may be integrated into licensure requirements, for example, as part of what facilities must demonstrate in their application. They also may be a more general part of state regulations governing operating requirements, along with staffing, placement, and other standards. They may be as simple as requiring information at licensure and the development and maintenance of policies and procedures, or they may include detailed requirements regarding different areas of facility internal structure and oversight.
Requirements related to special populations. States identify a range of special populations for which they wish to target services. This is far truer of SUD treatment than mental disorder treatment and often stems from block grant requirements. The two most common populations identified, particularly for SUD residential treatment, are those with co-occurring M/SUDs and pregnant and parenting women or parents of dependent children. Regarding the latter, many states have specific requirements for residential facilities in which pregnant women, parenting women, and/or families with dependent children may receive treatment, including educational, health, and safety requirements for children.
Regarding standards applicable to treating those with co-occurring M/SUDs, although additional requirements may exist in contracts or policy documents, in the documentation reviewed we found nearly twice as many states with requirements for treatment of co-occurring M/SUD disorders stemming from the SUD side of state policy compared with mental disorder residential treatment (Figure 12). Many of the former reflect requirements based in Section 1115 waivers but states have, apart from that, often sought to ensure that SUD-focused treatment facilities address mental disorders as well. Reciprocity is lacking on the mental health side in more than half of all states.
| FIGURE 12. Number of States with Provisions for Treatment of Co-occurring Disorders Specific to Residential Treatment |
|---|
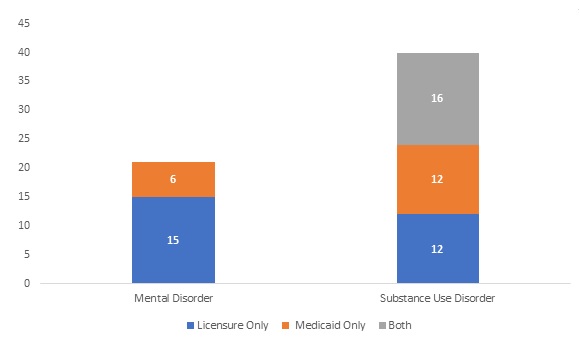 |
Other Key Findings
In addition to the conclusions drawn regarding specific domains above, at least three overarching findings warrant consideration.
First, there is good evidence that Section 1115 demonstrations, as well as the ASAM criteria, are critical to strengthening oversight of residential SUD treatment, although the requirements of the demonstrations have changed over time and are not uniform. The state structure and oversight of residential mental health treatment has not kept pace with change for residential SUD treatment. However, if more states obtain Section 1115 waivers that affect reimbursement of mental disorder treatment in IMDs rather than just SUD treatment, it is possible that similar strides could take place for mental disorder residential treatment.
Second, we were not able to include all facility types in this Compendium. For example, small group homes and recovery housing, where clinical treatment is not integrated into the residence, were excluded. These types of facilities may or may not be regulated or licensed. They may be providing very valuable benefits to their residents or may be providing services of unknown quality. A comprehensive understanding of these types of facilities requires more research and perhaps suggests a counterpart review of, for instance, recovery housing. Such a study could inform what oversight exists and what is lacking and, on the basis of the findings of the current study, help identify ways to improve the safety and quality of care in such facilities.
Third, states clearly have diverse ways of overseeing M/SUD treatment.
-
Some states rely heavily on published statutes and, even more so, on regulations to provide primary governance of M/SUD treatment, including residential treatment facilities.[154] This type of oversight results in clearly established and transparent requirements that lay out the legal basis for oversight and licensure. It also may result in requirements being established that can be difficult to change when flexibility or adaptation is needed, especially if rapid change is required. In addition, there may be instances in which events have changed how states wish to oversee facilities, but contradictory regulations may not yet be repealed. In these instances, practice may move ahead of regulatory requirements, generating unpredictability and possible confusion. Comparable to legally binding licensure and oversight requirements are state Medicaid statutes and regulations, as well as waiver documents or state plans that have been approved by CMS and, thereby, become binding on the state Medicaid agency and its agents and enrolled providers. Again, these binding Medicaid requirements have the benefit of transparency and certainty, provided rapid change is not required.
-
Some states rely more heavily on contractual requirements, also binding but often less transparent. These may include state Medicaid provider agreements, contracts by the state Medicaid agency with its MCEs or Administrative Service Organizations (ASOs), and contracts by Medicaid MCEs or ASOs with providers. In the nonMedicaid realm, this applies as well to contracts between the state and providers who are recipients of block grant or other state funds. Depending on the state, amending contract language may be less onerous than amending regulations. Sometimes these documents are readily available online; at other times, accessing this information can be difficult.
-
States also rely on agency licensing or standards manuals and, for Medicaid, provider manuals or other policy documents. Theoretically, these may be less binding on providers. However, many state statutes, regulations, or provider agreements expressly require compliance with such documents, and some explicitly incorporate these documents by reference into their regulations or other legal standards. This approach, especially if state regulations are not extensive, has the benefit of requiring only that the manual or other document be amended and published to alter requirements when doing so may be time sensitive. This assumes of course that state administrative procedure laws permit change to occur in this fashion. Additionally, when provider manuals are the province of Medicaid MCEs, enrollment as a provider often is required to obtain access to secure portals where manuals and other MCE policy documents are kept. Similarly, access to information about Medicaid provider enrollment and to the form of state Medicaid provider agreements may first require initiating an application to enroll. All of these hurdles limit our comprehensive understanding of state oversight of M/SUD residential treatment facilities and make public understanding of the system of behavioral health less than simple.
REFERENCES
-
The Joint Commission. Guide to Joint Commission Behavioral Health Care Accreditation. https://www.jointcommission.org/assets/1/18/2010_bhc_accreditation_guide_w_cov.pdf.
-
Centers for Medicare & Medicaid Services. New Service Delivery Opportunities for Individuals With a Substance Use Disorder. SMD #15-003. July 27, 2015. https://www.medicaid.gov/federal-policy-guidance/downloads/SMD15003.pdf.
-
Centers for Medicare & Medicaid Services. Strategies to Address the Opioid Epidemic. SMD #17-003. November 1, 2017. https://www.medicaid.gov/federal-policy-guidance/downloads/smd17003.pdf.
-
Centers for Medicare & Medicaid Services. Opportunities to Design Innovative Service Delivery Systems for Adults With a Serious Mental Illness or Children With a Series Emotional Disturbance. SMD #19-011. November 13, 2018. https://www.medicaid.gov/sites/default/files/federal-policy-guidance/downloads/smd18011.pdf.
-
For purposes of this Compendium, the term licensure is broadly used to include other terms such as certification, designation, or approval. In the state summaries, the terms actually used by each state are clear.
-
We use the term medication-assisted treatment (MAT), rather than medication treatment or medication for OUD, to refer to medication treatment for opioid or alcohol use disorder: (1) because that is the language used in state documents we reviewed; and (2) in order to maintain a distinction between medication for OUD or AUD treatment and medication for psychiatric or other disorders, including withdrawal management drugs that are not treatment for OUD or AUD.
-
Substance Abuse and Mental Health Services Administration. National Mental Health Services Survey (N-MHSS): 2017--Data on Mental Health Treatment Facilities. 2018. https://www.samhsa.gov/data/sites/default/files/cbhsq-reports/2017_National_Mental_Health_Services_Survey.pdf.
-
Authors' analysis of Substance Abuse and Mental Health Services Administration. National Mental Health Services Survey (N-MHSS): 2017. Data on Mental Health Treatment Facilities. 2018. https://www.samhsa.gov/data/sites/default/files/cbhsq-reports/2017_National_Mental_Health_Services_Survey.pdf.
-
Substance Abuse and Mental Health Services Administration. National Survey of Substance Abuse Treatment Services (N-SSATS): 2017. Data on Substance Abuse Treatment Facilities. 2018. https://www.samhsa.gov/data/sites/default/files/cbhsq-reports/2017_NSSATS.pdf.
-
Author's analysis of Substance Abuse and Mental Health Services Administration, National Survey of Substance Abuse Treatment Services (N-SSATS): 2017. Data on Substance Abuse Treatment Facilities. Rockville, MD: Substance Abuse and Mental Health Services Administration, 2018.
-
American Association for Community Psychiatry. Level of Care Utilization System for Psychiatric and Addiction Services. https://www.communitypsychiatry.org/resources/locus.
-
Stewart MT, O'Brien PL, Shields MC, White MC, Mulvaney-Day N. State Residential Treatment for Behavioral Health Conditions: Regulation and Policy Environmental Scan. Office of the Assistant Secretary for Planning and Evaluation; November 2019. https://aspe.hhs.gov/basic-report/state-residential-treatment-behavioral-health-conditions-regulation-and-policy-environmental-scan.
-
Medicaid and CHIP Payment and Access Commission. Report to Congress on Oversight of Institutions for Mental Diseases. December 2019. https://www.macpac.gov/publication/report-to-congress-on-oversight-of-institutions-for-mental-diseases/.
-
For purposes of this Compendium, the term licensure is broadly used to include other terms such as certification, designation, or approval. In the state summaries at Appendix B, the terms actually used by each state are clear.
-
For this reason and because, as noted above, other factors are involved in state oversight and licensure, none of this document should be taken to constitute legal advice.
-
Frank R, Glied S. Better But Not Well: Mental Health Policy in the United States Since 1950. Baltimore, MD: Johns Hopkins University Press; 2006.
-
For example, Minnesota Intensive Residential Treatment Services Variance R36V.01.
-
American Society of Addiction Medicine. The ASAM Criteria: Treatment Criteria for Addictive, Substance-Related, and Co-Occurring Conditions. 3rd ed. Rockville, MD: American Society of Addiction Medicine; 2013.
-
For example, District of Columbia residential mental health treatment facilities (see District of Columbia summary Appendix B).
-
For example, Wisconsin Admin. Code DHS § 75.01(2) (Community Substance Abuse Service Standards).
-
For example, Arkansas summary Appendix B.
-
For example, Minnesota summary Appendix B.
-
For example, 2 Code Colo. Regs. §§ 502-1.21.100, 502-1.21.120.3.C.
-
Reqirements for a CON historically have been used to ensure that operation of a proposed new facility meets the needs of the community.
-
For example, New York Comp. Codes R. & Regs. tit. 14, § 595.5(a) (MH certification).
-
For example, New Hampshire summary Appendix B.
-
For example, Massachusetts Gen. Laws ch. 105, § 164.012(A) (SU).
-
For example, 25 Texas Admin. Code §§ 448.403, 448.404, 448.407.
-
See Iowa summary Appendix B.
-
Mississippi Operational Standards for Mental Health, Intellectual/Developmental Disabilities, and Substance Use Disorders Community Service Providers § 16.5.
-
For example, Missouri Code Regs. Tit. 9, §§ 10-7.010, 10-7.030.
-
Sherman LJ, Lynch SE, Greeno CG, Hoeffel EM. Behavioral Health Workforce: Quality Assurance Practices in Mental Health Treatment Facilities. The CBHSQ Report. Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration; 2017.
-
Richardson J, Cowell A, Villeneuve E, Olmsted KR, Karon S, Whitter M, Trick M, Gray C, Fuller DB. Survey on Substance Use Disorder Patient Placement Criteria and Assessments: Final Report. Washington, DC: Office of the Assistant Secretary for Planning and Evaluation; in review.
-
For example, 14 CRR-NY 595.8.
-
For example, 175 Nebraska Admin. Code, ch. 19, § 006.09.
-
For example, New Hampshire Code Admin. R. He-P826.16.
-
For example, Minnesota Intensive Residential Treatment Services Variance R36V.04.
-
For example, Vermont DOH Preferred Providers: SUD Treatment Standards, § 17.2.2.
-
We do not include separate requirements related to MAT that are not integrated into the residential regulatory scheme.
-
For example, Minnesota Intensive Residential Treatment Services Variance R36V.08.
-
Substance Abuse and Mental Health Services Administration. Medicaid Coverage of Medication-Assisted Treatment for Alcohol and Opioid Use Disorders and of Medication for the Reversal of Opioid Overdose. HHS Publication No. SMA-18-5093. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2018.
-
For example, District of Columbia Mun. Regs. tit. 22, § 6331.5, 6332.6, 6333.6.
-
For example, District of Columbia Mun. Regs. tit. 22, § 6300.11.
-
See Idaho summary Appendix B.
-
For example, Delaware Adult Behavioral Health DHSS Service Certification and Reimbursement Manual, § 4.3.
-
Medicaid.gov. Behavioral health services. https://www.medicaid.gov/medicaid/benefits/behavioral-health-services/index.html.
-
Beronio K, Glied S, Frank R. How the Affordable Care Act and Mental Health Parity and Addiction Equity Act greatly expand coverage of behavioral health care. Journal of Behavioral Health Services & Research. 2014;41(4):410-28.
-
Priest K, Leof A, McCarty D, et al. Medicaid coverage for residential substance use disorder treatment: addressing the institution for mental disease exclusion policy. Health Affairs Blog. August 31, 2017. https://www.healthaffairs.org/do/10.1377/hblog20170831.061745/full/.
-
Melecki S, Weider K. The Medicaid Institution for Mental Diseases (IMD) Exclusion. Medicaid and CHIP Payment Access Commission; March 31, 2016. https://www.macpac.gov/wp-content/uploads/2016/03/The-Medicaid-Institution-for-Mental-Diseases-IMD-Exclusion.pdf.
-
Musumeci M, Chidambaram P, Orgera, K. State Options for Medicaid Coverage of Inpatient Behavioral Health Services. Kaiser Family Foundation; November 2019. http://files.kff.org/attachment/Report-Brief-State-Options-for-Medicaid-Coverage-of-Inpatient-Behavioral-Health-Services.
-
Musumeci M, Tolbert J. Federal Legislation to Address the Opioid Crisis: Medicaid Provisions in the SUPPORT Act. Kaiser Family Foundation; October 5, 2018. https://www.kff.org/medicaid/issue-brief/federal-legislation-to-address-the-opioid-crisis-medicaid-provisions-in-the-support-act/.
-
For example, Arkansas State Plan page 6c16 (July 1, 2017). https://medicaid.mmis.arkansas.gov/Download/general/units/ORP/ARMedicaidSP.pdf.
-
For example, Nebraska Medicaid Psychiatric Residential Rehabilitation Medicaid Service Definitions. http://dhhs.ne.gov/Behavioral%20Health%20Service%20Definitions/Psychiatric%20Residential%20Rehabilitation.pdf.
-
For example, Wyoming Department of Health Provider Manual. https://wymedicaid.portal.conduent.com/manuals/Manual_CMS1500_01_01_20.pdf.
-
In situations such as that in Wyoming, the state is treated as not regulating or enrolling the residential facility.
-
Centers for Medicaid & Medicaid Services. Medicaid.gov. State waivers list. https://www.medicaid.gov/medicaid/section-1115-demo/demonstration-and-waiver-list/index.html.
-
District of Columbia Behavioral Health Transformation Section 1115 demonstration approval. https://www.medicaid.gov/Medicaid-CHIP-Program-Information/By-Topics/Waivers/1115/downloads/dc/dc-behavioral-health-transformation-ca.pdf.
-
Vermont Global Commitment to Health Section 1115 SUD Implementation Protocol. https://www.medicaid.gov/Medicaid-CHIP-Program-Information/By-Topics/Waivers/1115/downloads/vt/vt-global-commitment-to-health-ca.pdf.
-
Michigan 1115 Pathway to Integration Section 1115 approved demonstration. https://www.medicaid.gov/Medicaid-CHIP-Program-Information/By-Topics/Waivers/1115/downloads/mi/mi-behavioral-health-ca.pdf.
-
Michigan Medicaid Provider Manual. http://www.mdch.state.mi.us/dch-medicaid/manuals/MedicaidProviderManual.pdf.
-
Maryland Medicaid summary Appendix B.
-
Kentucky HEALTH Section 1115 approved demonstration. https://www.medicaid.gov/Medicaid-CHIP-Program-Information/By-Topics/Waivers/1115/downloads/ky/ky-health-ca.pdf.
-
Nevada Medicaid Services Manual Chapter 400. http://dhcfp.nv.gov/uploadedFiles/dhcfpnvgov/content/Resources/AdminSupport/Manuals/MSM/C400/MSM_400_19_07_31.pdf.
-
Maine Medicaid Summary Appendix B.
-
New Hampshire Substance Use Disorder Treatment and Recovery Access Section 1115 demonstration approval. https://www.medicaid.gov/Medicaid-CHIP-Program-Information/By-Topics/Waivers/1115/downloads/nh/nh-sud-treatment-recovery-access-ca.pdf.
-
New Mexico Centennial Care 2.0 Section 1115 Medicaid Demonstration approval. https://www.medicaid.gov/Medicaid-CHIP-Program-Information/By-Topics/Waivers/1115/downloads/nm/nm-centennial-care-ca.pdf.
-
Washington Medicaid Transformation Project approved Section 1115 waiver. https://www.medicaid.gov/Medicaid-CHIP-Program-Information/By-Topics/Waivers/1115/downloads/wa/wa-medicaid-transformation-ca.pdf.
-
Healthy Indiana Section 1115 approved waiver. https://www.medicaid.gov/Medicaid-CHIP-Program-Information/By-Topics/Waivers/1115/downloads/in/in-healthy-indiana-plan-support-20-ca.pdf.
-
Maryland Health Choice approved Section 1115 waiver. https://www.medicaid.gov/Medicaid-CHIP-Program-Information/By-Topics/Waivers/1115/downloads/md/md-healthchoice-ca.pdf.
-
Massachusetts Health approved Section 1115 waiver. https://www.medicaid.gov/Medicaid-CHIP-Program-Information/By-Topics/Waivers/1115/downloads/ma/MassHealth/ma-masshealth-eval-desgn-2014-2017-01302016.pdf.
-
North Carolina Medicaid Reform Demonstration Section 1115 approved waiver. https://www.medicaid.gov/Medicaid-CHIP-Program-Information/By-Topics/Waivers/1115/downloads/nc/nc-medicaid-reform-ca.pdf.
-
TennCare II Section 1115 approved waiver. https://www.medicaid.gov/Medicaid-CHIP-Program-Information/By-Topics/Waivers/1115/downloads/tn/tn-tenncare-ii-ca.pdf.
-
For example, Indiana Sub-Acute Stabilization Facilities, 440 Ind. Admin. Code 7.5-4-7.
-
Maryland Summary Appendix B.
-
Substance Abuse and Mental Health Services Administration. Projections of National Expenditures for Treatment of Mental and Substance Use Disorders, 2010-2020. HHS Publication No. SMA-14-4883. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2014.
-
See state summaries for Illinois, Iowa, Kansas, Massachusetts, Ohio, Oregon, Washington, and Wisconsin in Appendix B.
-
Michigan State summary Appendix B.
-
Louisiana State summary Appendix B.
APPENDIX A. DETAILED TABLES
Acronyms
The following acronyms are mentioned in this appendix.
| ASAM | Americans Society of Addiction Medicine |
|---|---|
| CON | Certificate of Need |
| IDU | Injection Drug Use |
| IMD | Institution for Mental Disease |
| L/C | Licensure/Certification |
| MAT | Medication-Assisted Treatment |
| MH | Mental Health |
| QA/QI | Quality Assurance/Quality Improvement |
| PPW | Pregnant and Parenting Women |
| R/S | Restraint/Seclusion |
| Stds | Standards |
| SU | Substance Use |
| SUD | Substance Use Disorder |
| WM | Withdrawal Management |
Tables
| TABLE A25. Source of State Medicaid Authority to Reimburse Residential Mental Health Treatment in IMDs | |||
|---|---|---|---|
| State | Section 1115 IMD Waiver | "In Lieu of" Provisiona | DSH Paymentsa |
| Alabama | X | X | X |
| Alaska | X | X | ○ |
| Arizona | X | ○ | ○ |
| Arkansas | X | ○ | ○ |
| California | X | X | X |
| Colorado | X | ○ | X |
| Connecticut | X | X | ○ |
| DC | ● | ○ | ○ |
| Delaware | X | ○ | ○ |
| Florida | X | ○ | ○ |
| Georgia | X | X | X |
| Hawaii | X | ○ | X |
| Idaho | X | X | X |
| Illinois | X | ○ | ○ |
| Indiana | X | ○ | X |
| Iowa | X | ○ | X |
| Kansas | X | X | ○ |
| Kentucky | ● | ○ | ○ |
| Louisiana | X | ○ | ○ |
| Maine | X | X | ○ |
| Maryland | X | X | ○ |
| Massachusetts | ● | ○ | X |
| Michigan | X | ○ | ○ |
| Minnesota | X | ○ | ○ |
| Mississippi | X | ○ | X |
| Missouri | X | ○ | ○ |
| Montana | X | X | X |
| Nebraska | X | ○ | ○ |
| Nevada | X | ○ | X |
| New Hampshire | X | ○ | ○ |
| New Jersey | X | ○ | ○ |
| New Mexico | X | ○ | X |
| New York | X | ○ | ○ |
| North Carolina | X | X | ○ |
| North Dakota | X | X | ○ |
| Ohio | X | ○ | ○ |
| Oklahoma | X | X | ○ |
| Oregon | X | ○ | ○ |
| Pennsylvania | X | X | ○ |
| Rhode Island | X | ○ | X |
| South Carolina | X | ○ | ○ |
| South Dakota | X | X | ○ |
| Tennessee | X | ○ | X |
| Texas | X | ○ | ○ |
| Utah | X | ○ | X |
| Vermont | ● | X | X |
| Virginia | X | ○ | ○ |
| Washington | X | ○ | ○ |
| West Virginia | X | X | ○ |
| Wisconsin | X | ○ | X |
| Wyoming | X | X | X |
NOTES: ●: Present; ○: Present but undetermined if MH and/or SU or if residential and/or inpatient; X: Not Present.
|
|||
| TABLE A26. Source of State Medicaid Authority to Reimburse Residential SUD Treatment in IMDs | |||
|---|---|---|---|
| State | Section 1115 IMD Waiver | "In Lieu of" Provisiona | DSH Paymentsa |
| Alabama | X | X | X |
| Alaska | ● | X | ○ |
| Arizona | X | ○ | ○ |
| Arkansas | X | ○ | ○ |
| California | ● | X | X |
| Colorado | X | ○ | X |
| Connecticut | X | X | ○ |
| DC | ● | ○ | ○ |
| Delaware | ● | ○ | ○ |
| Florida | X | ○ | ○ |
| Georgia | X | X | X |
| Hawaii | X | ○ | X |
| Idaho | X | X | X |
| Illinois | ● | ○ | ○ |
| Indiana | ● | ○ | X |
| Iowa | X | ○ | X |
| Kansas | ● | X | ○ |
| Kentucky | ● | ○ | ○ |
| Louisiana | ● | ○ | ○ |
| Maine | X | X | ○ |
| Maryland | ● | X | ○ |
| Massachusetts | ● | ○ | X |
| Michigan | ● | ○ | ○ |
| Minnesota | ● | ○ | ○ |
| Mississippi | X | ○ | X |
| Missouri | X | ○ | ○ |
| Montana | X | X | X |
| Nebraska | ● | ○ | ○ |
| Nevada | X | ○ | X |
| New Hampshire | ● | ○ | ○ |
| New Jersey | ● | ○ | ○ |
| New Mexico | ● | ○ | X |
| New York | X | ○ | ○ |
| North Carolina | ● | X | ○ |
| North Dakota | X | X | ○ |
| Ohio | ● | ○ | ○ |
| Oklahoma | X | X | ○ |
| Oregon | ● | ○ | ○ |
| Pennsylvania | ● | X | ○ |
| Rhode Island | ● | ○ | X |
| South Carolina | X | ○ | ○ |
| South Dakota | X | X | ○ |
| Tennessee | X | ○ | X |
| Texas | X | ○ | ○ |
| Utah | ● | ○ | X |
| Vermont | ● | X | X |
| Virginia | ● | ○ | ○ |
| Washington | ● | ○ | ○ |
| West Virginia | ● | X | ○ |
| Wisconsin | ● | ○ | X |
| Wyoming | X | X | X |
NOTES: ●: Present; ○: Present but undetermined if MH and/or SU or if residential and/or inpatient; X: Not Present.
|
|||
APPENDIX B. SEPARATE STATE SUMMARIES
Acronyms
The following acronyms are mentioned in this appendix. Many acronyms have several meanings, usually due to being state agencies. All of the meanings are listed for that acronym.
| A&D | Alcohol and Drug |
|---|---|
| AAAHC | Accreditation Association for Ambulatory Health Care |
| AAS | American Association of Suicidology |
| ACHC | Accreditation Commission for Health Care |
| ACT | Assertive Community Treatment |
| ACU | Acute Crisis Unit |
| ADA | Americans with Disabilities Act |
| ADAP | Vermont Division of Alcohol and Drug Abuse Programs |
| ADL | Activity of Daily Living |
| AED | Automated External Defibrillator |
| AHCA | Florida Agency for Health Care Administration |
| AHCCCS | Arizona Health Care Cost Containment System Administration |
| AHS | Vermont Agency of Human Services |
| AIDS | Acquired Immunodeficiency Syndrome |
| ALOS | Average Length Of Stay |
| ALTCS | Arizona Long Term Care System |
| AMHR | Adult Mental Health Residential |
| AN | Anorexia Nervosa |
| ANSA | Adult Needs and Strengths Assessment |
| AOA | American Osteopathic Association |
| AODE | Alcohol and Drug Abuse Treatment Entity |
| APN | Advanced Nurse Practitioner |
| APRN | Advanced Practice Registered Nurse |
| APRTP | Acute Psychiatric Residential Treatment Program |
| ARNP | Advanced Registered Nurse Practitioner |
| ARTC | Adult Residential Treatment Center |
| ARTS | Virginia Addiction and Recovery Treatment Services |
| ASAM | Americans Society of Addiction Medicine |
| ASAM PPC-3 | ASAM Patient Placement Criteria for the Treatment of Substance-Related Disorders: Third Edition |
| ASI | Addiction Severity Index |
| ASO | Administrative Service Organization |
| ASRF | Adult Supportive Residential Facility |
| ATU | Acute Treatment Unit |
| BAC | Blood Alcohol Content |
| BCLS | Basic Cardiac Life Support |
| BDAS | New Hampshire Bureau of Drug and Alcohol Services |
| BH | Behavioral Health |
| BH-ASO | Behavioral Health Administrative Service Organization |
| BH-MCO | Behavioral Health Managed Care Organization |
| BHA | Behavioral Health Agency |
| Maryland Behavioral Health Administration | |
| BHC | Behavioral Health Center |
| BHCC | Behavioral Health Care Coordination |
| BHCN | Behavioral Health Community Network |
| BHCR | Behavioral Health Community Residence |
| BHDDH | Rhode Island Department of Behavioral Healthcare, Developmental Disabilities and Hospitals |
| BHMC | Hawaii Behavioral Health Managed Care |
| BHO | Behavioral Health Organization |
| Behavioral Healthcare Organization | |
| BHP | Connecticut Behavioral Health Partnership |
| BHRF | Behavioral Health Residential Facility |
| BHRP | Behavioral Health Recovery Program |
| BHS | Behavioral Health Service |
| BHSD | New Mexico Behavioral Health Services Division |
| BHSO | Behavioral Health Service Organization |
| BHSU | Behavioral Health Stabilization Unit |
| BMC | Behavior Management Committee |
| BMHS | New Hampshire Bureau of Mental Health Services |
| BMS | West Virginia Bureau for Medical Services |
| BN | Bulimia Nervosa |
| CAC | Certified Addition Counselor |
| CAP | Corrective Action Plan |
| CARF | Commission on Accreditation of Rehabilitation Facilities |
| CASII | Child and Adolescent Service Intensity Instrument |
| CBHP | Connecticut Behavioral Health Partnership |
| CBRF | Community-Based Residential Facility |
| CBSCC | Community-Based Structured Crisis Center |
| CCARC | Comprehensive Community Addiction Recovery Center |
| CCO | Coordinated Care Organization |
| CCS | Community Crisis Stabilization |
| CDC | Centers for Disease Control and Prevention |
| CDP | Chemical Dependency Professional |
| Chemical Dependency Program | |
| CDP-T | Chemical Dependency Professional Trainee |
| CDTF | Chemical Dependency Treatment Facility |
| CEO | Chief Executive Officer |
| CEDT | Certified Eating Disorder Treatment |
| CFR | Code of Federal Regulations |
| CIWA-Ar | Clinical Institute Withdrawal Assessment Alcohol scale Revised |
| CIWA-R | Clinical Institute Withdrawal Assessment Revised |
| CMHC | Community Mental Health Center |
| CMHRT | Community Mental Health Residential Treatment |
| CMS | Centers for Medicare & Medicaid Services |
| COA | Council on Accreditation of Services for Families and Children |
| CON | Certificate of Need |
| COPSD | Co-Occurring Psychiatric and Substance use Disorders |
| CPA | Certified Public Accountant |
| CPC | Comprehensive Primary Care |
| CPEP | Comprehensive Psychiatric Emergency Program |
| CPR | Cardiopulmonary Resuscitation |
| CPSW | Certified Peer Support Worker |
| CQL | Council on Quality Leadership |
| CRC | Crisis Receiving Center |
| CREDIT | Community Residence for Eating Disorder Integrated Treatment |
| CRS | Crisis Residential Services |
| CRT | Community Rehabilitation and Treatment |
| CSC | Crisis Service Center |
| CSRS | Crisis Stabilization Residential Services |
| CSS | Crisis Stabilization Services |
| CSSP | Community Support Specialist |
| CSTAR | Comprehensive Substance Treatment And Rehabilitation |
| CSU | Crisis Stabilization Unit |
| CTC | Crisis Triage Center |
| DATA 2000 | Drug Addiction Treatment Act of 2000 |
| DBH | Alaska Division of Behavioral Health |
| District of Columbia Department of Behavioral Health | |
| Idaho Division of Behavioral Health | |
| New Hampshire Division of Behavioral Health | |
| Wyoming Division of Behavioral Health | |
| DBHDD | Georgia Department of Behavioral Health and Developmental Disabilities |
| DBHDID | Kentucky Department for Behavioral Health, Developmental and Intellectual Disabilities |
| DBHDS | Virginia Department of Behavioral Health and Developmental Services |
| DCF | Florida Department of Children and Families |
| DCH | Georgia Department of Community Health |
| DCP | Diversion Control Plan |
| DDAP | Pennsylvania Department of Drug and Alcohol Programs |
| DDC | Dual Diagnosis Capable |
| DDCAT | Dual Diagnosis Capability in Addiction Treatment |
| DDE | Dual Diagnosis Enhanced |
| DDMHS | Vermont Department of Developmental and Mental Health Services |
| DHCF | District of Columbia Department of Health Care Finance |
| DHCFP | Nevada Division of Health Care Financing and Policy |
| DHCS | Alaska DHSS Division of Health Care Services |
| California Department of Health Care Services | |
| DHEC | South Carolina Department of Health and Environmental Control |
| DHHR | West Virginia Department of Health and Human Resources |
| DHHS | Maine Department of Health and Human Services |
| Michigan Department of Health and Human Services | |
| Nebraska Department of Health and Human Services | |
| New Hampshire Department of Health and Human Services | |
| North Carolina Department of Health and Human Services | |
| South Carolina Department of Health and Human Services | |
| DHI | New Mexico Division of Health Improvement |
| DHS | Arkansas Department of Human Services |
| Hawaii Department of Human Services | |
| Illinois Department of Human Services | |
| Iowa Department of Human Services | |
| Minnesota Department of Human Services | |
| New Jersey Department of Human Services | |
| North Dakota Department of Human Services | |
| Pennsylvania Department of Human Services | |
| Utah Department of Human Services | |
| Wisconsin Department of Health Services | |
| DHSR | North Carolina Division of Health Service Regulation |
| DHSS | Alaska Department of Health and Social Services |
| Delaware Department of Health and Social Services | |
| Missouri Department of Health and Senior Services | |
| DLRA | Michigan Department of Licensing and Regulatory Affairs |
| DMAS | Virginia Department of Medical Assistance Services |
| DMC-ODS | Drug Medi-Cal Organized Delivery System |
| DME | Durable Medical Equipment |
| DMH | Alabama Department of Mental Health |
| Illinois Division of Mental Health | |
| Massachusetts Department of Mental Health | |
| Mississippi Department of Mental Health | |
| Missouri Department of Mental Health | |
| DMHA | Indiana Division of Mental Health and Addiction |
| DMHAS | Connecticut Department of Mental Health and Addiction Services |
| Ohio Department of Mental Health and Addiction Services | |
| DMHDDSAS | North Carolina Division of Mental Health, Developmental Disabilities, and Substance Abuse Services |
| DMHSAS | Tennessee Department of Mental Health and Substance Abuse Services |
| DMS | Kentucky Department for Medicaid Services |
| DOH | Hawaii Department of Health |
| New Mexico Department of Health | |
| Ohio Department of Health | |
| South Dakota Department of Health | |
| Utah Department of Health | |
| Washington State Department of Health | |
| Wyoming Department of Health | |
| DPBH | Nevada Division of Public and Behavioral Health |
| DPH | Connecticut Department of Public Health |
| Illinois Department of Public Health | |
| Iowa Department of Public Health | |
| Massachusetts Department of Public Health | |
| DPHE | Colorado Department of Public Health and Environment |
| DPHHS | Montana Department of Public Health and Human Services |
| DSAMH | Delaware Division of Substance Abuse and Mental Health |
| Utah Division of Substance Abuse and Mental Health | |
| DSH | Disproportionate Share Hospital |
| DSHP | Designated State Health Program |
| DSM | Diagnostic and Statistical Manual of Mental Disorders |
| DSRIP | Delivery System Reform Incentive Payment |
| DSS | California Department of Social Services |
| Missouri Department of Social Services | |
| South Dakota Department of Social Services | |
| DTA | Massachusetts Department of Transitional Assistance |
| DUI | Driving Under the Influence |
| E&T | Evaluation and Treatment |
| EDNOS | Eating Disorder Not Otherwise Specified |
| EDTP | Eating Disorder Treatment Plan |
| EOU | Extended Observation Unit |
| EQR | External Quality Review |
| EQRO | External Quality Review Organization |
| ESMI | Early Serious Mental Illness |
| FBCS | Facility Based Crisis Stabilization |
| FDA | Food and Drug Administration |
| FEP | First Episode Psychosis |
| FFP | Firm Fixed Price |
| FFS | Fee-For-Service |
| FPL | Federal Poverty Level |
| FS | Florida Statutes |
| FSTRA | Forensic Supervised Transitional Residential and Aftercare Facility |
| FTE | Full-Time Equivalent |
| GAIN-I | Global Appraisal of Individual Needs Initial |
| GAIN-SS | Global Appraisal of Individual Need-Short Screen |
| GED | General Educational Development |
| HCA | Washington State Health Care Authority |
| HCPF | Colorado Department of Health Care Policy and Financing |
| HEDIS | Healthcare Effectiveness Data and Information Set |
| HFR | Georgia Division of Healthcare Facility Regulation |
| HHSC | Texas Health and Human Services Commission |
| HHTF | Alcohol and Drug Halfway House Treatment Facility |
| HIV | Human Immunodeficiency Virus |
| HSD | New Mexico Human Services Department |
| Oregon Health Systems Division | |
| HUM | High Utilizer Management |
| IADL | Instrumental Activity of Daily Living |
| IBSER | Intensive Behavioral Support and Educational Residence |
| ICC | Intensive Care Coordination |
| ICD | International Classification of Diseases |
| ICF/PMI | Intermediate Care Facilities for Persons with a Mental Illness |
| IDD | Intellectual and Developmental Disability |
| IDDT | Integrated Dual Diagnosis Treatment |
| IDEA | Iowa Department of Inspections and Appeals |
| IDHW | Idaho Department of Health and Welfare |
| IDI | Initial Diagnostic Interview |
| IDT | Interdisciplinary Team |
| IHP | Individualized Habilitation Plan |
| IIS | Intensive Inpatient Services |
| IMD | Institution for Mental Disease |
| IMR | Illness Management and Recovery |
| IMS | Incidental Medical Services |
| IPC | Individual Plan of Care |
| IPP | Individual Program Plan |
| IPU | Inpatient Hospice Unit |
| IRP | Individualized Recovery/Resiliency Plan |
| IRRF | Intensive Residential Recovery Facility |
| IRTS | Intensive Residential Treatment Services |
| ISP | Individualized Service Plan |
| ITP | Individual Treatment Plan |
| IV | Intravenous |
| JCAHO | Joint Commission on Accreditation for Healthcare Organizations |
| KDADS | Kansas Department for Aging and Disability Services |
| KDHE | Kansas Department of Health and Environment |
| KFF | Kaiser Family Foundation |
| LAC | Licensed Addiction Counselor |
| LADC | Licensed Alcohol and Drug Counselor |
| LAR | Legally Authorized Representative |
| LBHA | Local Behavioral Health Authority |
| LBHC | Licensed Behavioral Health Center |
| LBHP | Licensed Behavioral Health Practitioner |
| LCSW | Licensed Certified Social Worker |
| LDH | Louisiana Department of Health |
| LGPC | Licensed Graduate Professional Counselor |
| LGSW | Licensed Graduate Social Worker |
| LICSW | Licensed Independent Clinical Social Worker |
| LIMHP | Licensed Independent Mental Health Practitioner |
| LIP | Licensed Independent Practitioner |
| LME | Local Management Entity |
| LMFT | Licensed Marriage and Family Therapist |
| LMHC | Licensed Mental Health Counselor |
| LMHP | Licensed Mental Health Professional |
| Licensed Mental Health Practitioner | |
| LMSW | Licensed Master Social Worker |
| LOC | Level of Care |
| LOCUS | Level of Care Utilization System |
| LPC | Licensed Professional Counselor |
| LPHA | Licensed Practitioner of the Healing Arts |
| LPN | Licensed Practical Nurse |
| LTR | Long-Term Resident |
| LTSR | Long-Term Structured Residence |
| LTSS | Long-Term Services and Supports |
| LVN | Licensed Vocational Nurse |
| MAT | Medication-Assisted Treatment |
| MCA | Montana Code Annotated |
| MCE | Managed Care Entity |
| MCO | Managed Care Organization |
| MCP | Managed Care Plans |
| MD | Medical Doctor |
| MDH | Maryland Department of Health |
| MH | Mental Health |
| MHA | Mental Health Agency |
| MHP | Mental Health Plan |
| Mental Health Professional | |
| MHPRR | Mental Health Psychiatric Rehabilitative Residence |
| MHPRR-As | Supportive Mental Health Psychiatric Rehabilitative Residence Apartment |
| MHRT | Mental Health Rehabilitation Technician |
| MHRTF | Mental Health Residential Treatment Facility |
| MLADC | Master Licensed Alcohol and Drug Counselor |
| NAC | Nevada Administrative Code |
| NCQA | National Committee on Quality Assurance |
| NMAP | Nebraska Medical Assistance Program |
| NMMCP | Nebraska Medicaid Managed Care Program |
| NOS | Not Otherwise Specified |
| NP | Nurse Practitioner |
| NRS | Nevada Revised Statutes |
| NTP | Narcotic Treatment Program |
| OADAP | Illinois Office of Alcohol and Drug Abuse Prevention |
| OASAS | New York State Office of Addiction Services and Supports |
| OBH | Colorado Office of Behavioral Health |
| Louisiana Office of Behavioral Health | |
| OCN&L | New Jersey Office of Certificate of Need and Licensure |
| ODASL | Oklahoma Determination of ASAM Service Level |
| ODM | Ohio Department of Medicaid |
| ODMHSAS | Oklahoma State Board of Mental Health and Substance Abuse Services |
| OHA | Oregon Health Authority |
| OHCA | Oklahoma Health Care Authority |
| OHFLAC | West Virginia Office of Health Facility Licensure and Certification |
| OHHS | Massachusetts Executive Office of Health and Human Services |
| OIG | Office of Inspector General |
| OMH | New York State Office of Mental Health |
| ORS | Oregon Revised Statutes |
| OSHA | Occupational Safety and Health Administration |
| OTP | Opioid Treatment Program |
| OUD | Opioid Use Disorder |
| PA | Physician Assistant |
| PACT | Program for Assertive Community Treatment |
| PCNS | Psychiatric Clinical Nurse Specialist |
| PCPP | Primary Care Physician Program |
| PIHP | Prepaid Inpatient Health Plan |
| PITF | Private Intermediate Treatment Facility |
| PMHP | Prepaid Mental Health Plan |
| PNMI | Private Non-Medical Institution |
| POC | Plan of Correction |
| PPC | Patient Placement Criteria |
| PRCSS | Psychiatric Residential Crisis Stabilization Services |
| PRTF | Psychiatric Residential Treatment Facility |
| QA | Quality Assurance |
| QAPI | Quality Assessment and Performance Improvement |
| QBHE | Qualified Behavioral Health Entity |
| QCC | Qualified Credential Counselor |
| QI | Quality Improvement |
| QMHP | Qualified Mental Health Professional |
| QMHP-CS | Qualified Mental Health Professional-Community Services |
| QSAP | Qualified Substance Abuse Professional |
| RARS | New York Residential Addiction Rehabilitative Services |
| RAS | Residential Adult Services |
| RCF | Residential Care Facility |
| RCF/PMI | Residential Care Facility for Persons with a Mental Illness |
| RCS | Residential Crisis Service |
| RDF | Alcohol and Drug Residential Detoxification Treatment Facility |
| RDS | Regional Detoxification Specialist |
| RH | Recovery House |
| RLD | Regulation and Licensing Department |
| RN | Registered Nurse |
| RRS | Recovery and Rehabilitation Support |
| Residential Rehabilitation Services | |
| RRTF | Alcohol and Drug Residential Rehabilitation Treatment Facility for Adults |
| RTF | Residential Treatment Facility |
| RTH | Residential Treatment Home |
| RTPF | Residential Treatment Program Facility |
| RTRF | Residential Treatment and Rehabilitation Facility |
| SA | Substance Abuse |
| SAMHSA | Substance Abuse and Mental Health Services Administration |
| SAPT | Substance Abuse Prevention and Treatment |
| SAPTA | Nevada Substance Abuse Prevention and Treatment Agency |
| SATF | Substance Abuse Treatment Facility |
| SBS | Specialized Behavior Support plan |
| SED | Serious Emotional Disturbance |
| SMI | Serious Mental Illness |
| SRF | Social Rehabilitation Facility |
| SFP | Social Rehabilitation Program |
| SMHPRR | Specialized Mental Health Psychiatric Rehabilitative Residence |
| SMHRF | Specialized Mental Health Rehabilitation Facility |
| SMI | Serious Mental Illness |
| SOD | Statement of Deficiency |
| SOTA | State Opioid Treatment Authority |
| SPMI | Serious and Persistent Mental Illness |
| SRT | Short-term Residential Treatment |
| SRTF | Secure Residential Treatment Facility |
| SSA | Substance Abuse Agency |
| SSDI | Social Security Disability Insurance |
| SSI | Supplemental Security Income |
| STD | Sexually Transmitted Disease |
| STF | Special Treatment Facility |
| SUD | Substance Use Disorder |
| SUD-BHP | Alaska Substance Use Disorder and Behavioral Health Program |
| TB | Tuberculosis |
| TC | Therapeutic Community |
| TCM | Transitional Case Management |
| TEDS | Treatment Episode Data Set |
| Temp Ob | Temporary Observation |
| THHS | Texas Health and Human Services |
| TIP | Treatment Improvement Protocol |
| TJC | The Joint Commission on Accreditation for Healthcare Organizations |
| TLP | Therapeutic Living Program |
| TLU | Transitional Living Unit |
| TRBHA | Arizona Tribal Regional Behavioral Health Authority |
| TSS | Transitional Support Services |
| UAP | Unlicensed Assistive Personnel |
| UM | Utilization Management |
| UP | Unlicensed Professional |
| WCRTS | Women and Children's Residential Treatment Services |
| WI-UPC | Wisconsin Uniform Placement Criteria |
| WM | Withdrawal Management |
| WDM | Withdrawal Management |
| WRAP | Wellness Recovery Action Plan |
| WTRS | Women's Treatment and Recovery Support |
| YAT | Young Adult in Transition Facility |
State Summaries
These profiles are available as separate PDFs:
APPENDIX C. DETAILED METHODOLOGY
Acronyms
The following acronyms are mentioned in this appendix.
| CHIP | Children's Health Insurance Program |
|---|---|
| M/SUD | Mental and Substance Use Disorders |
| MACPAC | Medicaid and CHIP Payment and Access Commission |
| MCE | Managed Care Entity |
Methodology
As a precursor to the collection and synthesis of data drawn primarily from state law, we conducted an environmental scan and interviewed experts in the field. The environmental scan summarizes the literature on oversight of residential care for M/SUDs in the United States. A systematic approach was used to conduct the environmental scan in which we examined national surveys, English-language peer-reviewed literature (2014-2018), and grey literature no more than 5 years old, unless identified as key by a subject matter expert. We conducted keyword searches using databases such as PubMed and Google Scholar. Relevant articles and other source documents were reviewed, synthesized, and summarized in the environmental scan, which is published separately.[1] In addition, we identified and interviewed a number of subject matter experts who are recognized in the acknowledgments section of this Compendium.
On the basis of findings from the environmental scan[1] and interviews with experts, we developed a template that provided the coding structure for data collected throughout the project. We gathered source data for all states by reviewing statutes and regulations governing M/SUD treatment and licensing or certification. We trained four analysts in both data collection and coding according to a standardized protocol. Senior members of the team worked closely with the analysts as they proceeded through the data collection to ensure completeness and relevance and verified the reliability and validity of coding done during the project. Relevant statutes and regulations from 51 jurisdictions were reviewed and abstracted into the data collection template. A senior staff person reviewed 25% of abstractions for completeness and accuracy. Any discrepancies among coders were discussed and adjudicated. We prepared detailed state summaries of: (1) licensure standards; and (2) Medicaid requirements by synthesizing the abstracted information (see Appendix B).
Throughout the study, we used a legal mapping framework. This approach provides structured steps to follow in reviewing and compiling information from legal documents. In addition, we coordinated with other federal efforts on this topic and leveraged efficiencies available through ongoing parallel efforts, such as those being led by the MACPAC.[2] By integrating input from leaders in this field throughout the course of the project, as well as applying a rigorous legal mapping framework for abstraction and synthesis, we generated accurate information to disseminate widely and inform next steps in addressing capacity for M/SUD treatment across the continuum of care.
The state summaries that resulted from data collection regarding licensure were shared with the individual states for validation. On the basis of input from those states, we revised the summaries as necessary. In some instances, state personnel provided additional sources of information beyond the statutes and regulations and, to the extent it was pertinent to the study, that information was included. Among other things, these additional sources of information sometimes included certification or licensure manuals and written input from state staff. All publicly available documents on which we relied are referenced in the state summaries.
In the summaries of state Medicaid requirements, we primarily relied on state Medicaid regulations and Section 1115 demonstration documents. Where necessary, these were supplemented with additional sources. The relative absence of certain requirements in state Medicaid regulations, however, does not mean that Medicaid programs do not have service requirements in provider agreements with Medicaid or Medicaid MCEs, provider manuals, or elsewhere. Similarly, some states may more passively rely on the presence of licensure requirements to ensure that service standards are in place.
During validation of the summaries of state licensing requirements, states sometime highlighted issues that required consistent resolution. For example, validating staff sometimes indicated that regulations were under review for amendment. In those cases, we adhered to the regulations in place at the time of review. Similarly, when a state indicated that its regulations were out of date and did not reflect the actual processes used by the state, but where the regulations had not been amended to reflect that reality, we maintained the summary so as to capture the actual regulatory status at the time of review. However, when states simply modified summaries, those changes were accepted unless they would have included information outside the scope of the summary. Additionally, to the extent that statutes and regulations had not been amended to reflect shifts in agencies responsible for oversight or licensure, we accepted the input of the agency and included the current names of agency(ies) responsible, rather than a prior agency that was still reflected in the language of the licensing laws.
Several parameters were placed around the scope of data collection to ensure consistency:
-
Residential treatment was defined as clinical treatment services provided in a 24-hour living environment. This definition generally eliminated programs such as group homes, halfway houses, recovery housing, or intoxication monitoring facilities, unless state statutes or regulations clearly indicated that clinical treatment must be provided by the facility. A facility that offered only supportive, life skills, or personal care-focused services was excluded from the scope of this study, although those services clearly have value in the treatment of M/SUDs. The exception to this exclusion relates to withdrawal management or detoxification facilities, some of which are not required to offer psychosocial counseling. Because some of these facilities do require such services and most incorporate some level of medical monitoring or care, we included them to the extent that the services are residentially based.
-
Only residential treatment facilities for adults were included; thus, treatment specific to children or adolescents was excluded. In practice, this means that we excluded psychiatric residential treatment facilities and other facilities intended to serve individuals below age 21 years.
-
We excluded facilities that are associated with the criminal justice system or that are in inpatient settings.
-
We examined state Medicaid separately in this Compendium. To the extent, however, that licensing standards apply only to publicly-funded residential treatment facilities, they are included even if Medicaid is within the definition of publicly-funded. This approach permitted us to capture requirements related to facilities that are recipients of block grant and/or other governmental funding. Uniquely Medicaid-related requirements are included in a separate summary for each state.
Study limitations. To fully understand a state's oversight of residential treatment facilities, one must examine more than the state statutes and regulations, which provide only a partial picture of how oversight works in reality. Those statutes and regulations are, however, the legally enforceable mechanisms that govern facilities, and they are publicly available to all stakeholders. In addition to statutes and regulations, states may rely on: (1) agency policy documents, such as manuals or guidance; (2) contracts with providers who receive public funding, such as from block grant funds; and (3) to the extent that Medicaid is considered, a separate set of regulations, agency policy documents, contracts with providers or MCEs, and requirements of federal Medicaid state plan amendments and waivers or demonstrations. In addition, one must understand the actual practices of the overseeing or licensing agency to appreciate how regulations are enforced, or not enforced, in reality. Absent interviews with state staff or other stakeholders, this Compendium cannot capture the latter.
Another limitation is that the summaries reflect state law at a single point in time. Statutes and regulations clearly are amended on an ongoing basis. This means that, at the point of publication of this Compendium, some statutes and regulations will have been amended, repealed, or replaced, rendering some portion of the summaries no longer accurate. For this reason and because, as noted above, other factors are involved in state oversight and licensure, none of this document should be taken to constitute legal advice.
Finally, the specific domains identified for data collection were selected to allow us to better understand the extent of regulatory oversight for residential treatment in each state. This involved deliberate selection of some characteristics and nonselection of others. For example, one important part of residential treatment regulation and oversight that we did not include was physical safety standards such as building, fire, and zoning requirements.
References
-
Stewart MT, O'Brien PL, Shields MC, White MC, Mulvaney-Day N. State Residential Treatment for Behavioral Health Conditions: Regulation and Policy Environmental Scan. Washington, DC: Office of the Assistant Secretary for Planning and Evaluation; November 2019. https://aspe.hhs.gov/system/files/pdf/262961/BehHeaConLR.pdf.
-
Medicaid and CHIP Payment and Access Commission. Report to Congress on Oversight of Institutions for Mental Diseases. December 2019. https://www.macpac.gov/publication/report-to-congress-on-oversight-of-institutions-for-mental-diseases/.